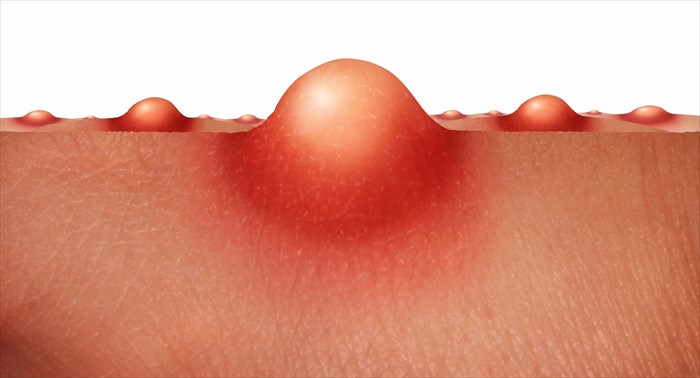
Infectious folliculitis
Bacterial Folliculitis
1. Staphylococcal folliculitis
Bockhart impetigo”. It is caused by the bacterium, staphylococcus aureus, and presents as pustules (most often without symptoms of fever). A person who develops folliculitis as a result of this bacterium is more often than not a chronic carrier (i.e. the bacterium is present in the system but does not present noticeable symptoms). For the most part, this bacterium is generally present on the skin but typically becomes problematic once it has entered the body via a wound (like a cut or open sore). For some, this is how they become a carrier.
A common form of bacterial folliculitis is barber’s itch, also known as pseudofolliculitis barbae (razor bumps / razor-burn folliculitis) which affects men with particularly course and curly beard hairs. When these hairs are cut short while shaving, regrowth tends to curve back into the skin causing ingrown hairs and resulting in inflammation, especially on the neck. Excessive close shaving can also trap small hairs beneath the surface of the skin, resulting in inflammation. Tiny cuts which occur during shaving allow opportunity for bacterial entry, causing damage to hair follicles.
This type of razor-burn folliculitis may also affect women who shave their legs. Those who frequently go for bikini waxes can also experience this form of folliculitis, but in their groin area. Dark, raised scars (keloids) can occur in either instance.
2. Gram-negative folliculitis
A variety of gram-negative bacteria cause this condition, each with their own symptoms. One of the most common forms is hot tub folliculitis (or pseudomonas folliculitis), as a result of an infection with pseudomonas aeruginosa bacterium. The name stems from the most likely source of contraction, inadequately sanitised spa baths or hot tubs, as well as heated pools with unregulated chlorine and pH levels. Red spots (without pus) and pustules which appear within 72 hours are common symptoms of this type of folliculitis. Aeromonas hydrophila bacterium may also cause folliculitis if you are exposed to it during recreational water activities.
A rare acne-like condition due to infection with Enterobacter, Klebsiella or Proteus gram-negative bacteria may occur in those with rosacea or acne vulgaris (2) as a direct result of long-term antibiotic treatment for these conditions. Eruptions are common in the facial area and present as pustules or pus-filled cysts (in 20% of patients), which normally clear once treatment has been discontinued.
Fungal Folliculitis
Second to S.Aureus bacteria, fungi are common culprits in the development of folliculitis.
1. Dermatophyte folliculitis
This form of the condition is caused by one of three types of fungus, namely the Epidermophyton, Microsporum or Trichophyton species. A fungal infection of the scalp affecting the hair follicles on the head commonly causes tinea capitis (or ringworm of the scalp) while this type of infection involving the beard and moustache is referred to as tinea barbae.
2. Malassezia (Pityrosporum) folliculitis
Many of the Malassezia species cause folliculitis. These yeasts occur naturally on the skin of health individuals and form part of the natural skin florae. Colonisation is exacerbated due to increased sebaceous gland activity (especially during adolescence), warm, humid climates and occasionally certain medication use (antibiotics, corticosteroids or immunosuppressants).
3. Candida folliculitis
Another opportunistic yeast pathogen, candida albicans can also provoke a folliculitis breakout within skinfolds or along the beard area of the face.
Viral folliculitis
1. Herpes folliculitis
This form of folliculitis is rare, and usually attributed to an infection with the varicella zoster virus (VZC). However, the herpes simplex viruses (HSV-1 or oral herpes and HSV-2 – genital herpes) can sometimes lead to a folliculitis breakout, most commonly in men with localised infections, which is also aggravated by shaving. The herpes zoster virus (responsible for shingles) and molluscum contagiosum can also lead to the formation of folliculitis pustules or papules (and crusted spots).
Demodex folliculitis
A microscopic hair follicle mite called demodex can lead to demodex folliculitis. Symptoms are clinically similar to that of another inflammatory skin condition, called rosacea. This form of folliculitis is most common among those with suppressed immune systems (which can occur due to a medical condition or as a side-effect of medication used for medical treatment).
Scabies, a highly contagious and itchy skin condition which develops due to an infestation of mites (Sarcoptes scabiei) can also provoke folliculitis symptoms (bumps), along with papules (swelling on the skin / small pimple), and vesicles (small fluid-filled cyst).
Environmental causes of folliculitis
1. Mechanical folliculitis
One example of the mechanical causes of this type of folliculitis is that of 
2. Occlusion folliculitis
Some topical products like adhesives (such as plasters for wound coverage), moisturisers, ointments, greases and oils can cause blockages of the skin and hair follicles, resulting in inflammation. The skin begins to swell at the opening of the hair follicle, causing occlusion folliculitis.
3. Chemical folliculitis
Other topical products, like coal tars and medications such as corticosteroids, also result in hair follicle inflammation due to blockage. This causes chemical folliculitis. Similarly, drug-induced folliculitis occurs as a result of oral medications including androgenic hormones, lithium, oral corticosteroids, some anticonvulsants and epidermal growth factor receptor inhibitors.
Skin conditions as causes of folliculitis
Many common skin problems involve the hair follicle which is often a primary mechanism of the disease process. Examples include acne, acne nuchae keloidalis (which produces pustules and keloid-like scars), lichen planus (a chronic rash and small raised bumps), lupus erythematosus and folliculitis decalvans (a form of alopecia which involves hair loss related scarring).
Conditions whereby inflammation and potential scarring occur due to follicular occlusion (inflammation and hair follicle blockage) include:
- Acne conglobata: A severe albeit uncommon form of acne which presents inflammatory nodulocystic bumps (burrowing and interconnecting abscesses) resulting in keloidal and atrophic scars. Scarring can result in considerable disfigurement.
- Dissecting cellulitis (or perifolliculitis capitis abscedens et suffodiens or Hoffman disease): A rare, but also severe and chronic inflammatory scalp disorder (which is a variation of scalp folliculitis) and results in significant scarring.
- Hidradenitis suppurativa: An infection and inflammation of the sweat glands (often in the armpits or groin areas) can result in this severe acne-like condition. Folliculitis-like bumps which develop in skin folds can lead to scarring once inflammation has cleared.
- Pilonidal sinus: In the cleft where the buttocks separate, an abscess-like pilonidal cyst containing hair, debris and dirt may form around the hair follicles. The formation can cause significant pain and become infected, oozing pus and sometimes blood, which produces a foul odour.
Forms of folliculitis with unclear (non-specific) causes
- Eosinophilic folliculitis (also known as Eosinophilic pustular folliculitis and Ofuji disease): Commonly affecting the head and neck areas, itchy bumps resembling a pustular rash can occur. It is believed that some breakouts are associated with immune suppression (either as a result of immunosuppressive medications or certain medical conditions, such as poorly controlled HIV or late stage AIDS). The condition causes intense and recurrent symptoms, as well as hyperpigmentation (dark skin patches).
- Buttock folliculitis: It is believed that this form of folliculitis may be a type of localised acne which presents acutely painful pustules on the buttocks. The condition can also become chronic, requiring topical treatment. Acute breakouts may be resolved with oral antibiotics. Buttock folliculitis can affect both males and females.
Folliculitis classifications
- Superficial folliculitis: This classification type involves part of a hair follicle. Superficial folliculitis usually includes bacterial (staphylococcus aureus, hot tub, razor bumps) and yeast infection (pityrosporum folliculitis) breakout forms of the condition.
- Deep folliculitis: This classification type involves the entire hair follicle and presents more severe symptoms. Deep folliculitis usually includes sycosis barbae (Barber’s itch), gram-negative folliculitis, eosinophilic folliculitis, and instances where hair follicles become deeply infected and present painful and swollen boils / furuncles (and carbuncles / clusters of boils – which may rupture and drain).
What are the main risk factors for folliculitis?
Anyone may develop some form of folliculitis during their lifetime. It is most likely that we all experience this condition to some extent, at some point.
Certain factors can contribute to susceptibility. Some of these include:
- Existing skin conditions, such as dermatitis and acne
- Medication treatment for acne or rosacea (i.e. the use of steroidal creams or long-term oral antibiotics)
- Existing medical conditions which present reduced resistance to infections (HIV/AIDS, diabetes and chronic leukaemia are some examples) and result in weakened immune systems.
- Perspiring excessively (hyperhidrosis)
- Men with curly hair who shave regularly (curly hair increases the incidence of ingrown hairs)
- Individuals who regularly shave or wax (this increases the risk of damage or injury to hair follicles)
- The regular wear of tight clothing styles (e.g. skinny jeans), or fabrics which trap perspiration and heat (e.g. high boots or rubber gloves) and may cause friction with the skin and hair beneath
- Regular use of spa baths and hot tubs, or swimming pools that aren’t maintained with chlorine
- Individuals who regularly use or work with substances that clog up hair follicles on the skin (e.g. tar, motor oil, cosmetics and make-up products)
Is folliculitis contagious?
Some infectious agents (bacteria) which cause folliculitis can be contagious – meaning that infection can be passed from one person to another. Means of transmission include skin-to-skin contact, the sharing of personal items such as razors or towels, or using hot tubs, Jacuzzis and spa baths that have been used by others with the infection.
Just about all instances of folliculitis, no matter what the underlying cause, are treatable, and thus can be cured. It is fairly rare for chronic / recurring conditions not to be resolved with appropriate treatment. For the most part, mild cases of folliculitis resolve on their own. More persistent instances may require some medical intervention which involves the taking or use of oral or topical medication/ointments.
References:
1. The Australasian College of Dermatologists. Folliculitis: https://www.dermcoll.edu.au/atoz/folliculitis/ [Accessed 09.11.2017]
2. Directory of Open Acess Journals. 2011. Gram-negative folliculitis. A rare problem or is it underdiagnosed? Case report and literature review: https://doaj.org/article/1c09c152c73e4c7fa48ccc0455fc4fc5 [Accessed 03.12.2017]