The World Health Organization (WHO) keeps a close eye on the many health conditions and diseases causing a global burden, especially those of the infectious variety, including Tuberculosis (TB).
The organisation frequently releases reports on the status of infectious diseases like TB releasing updated statistics and figures, for both world leaders and the public at large. Next on their agenda is to stress the urgency required for further action.
This year’s updated statistic report from WHO - Global Tuberculosis Report 2018 (1) – focusses on achievements made thus far and also makes the path ahead very clear – there are still enormous strides to be made and mountains to climb.
A global status report on the disease has been compiled every year since 1997. This year’s report was made publicly available on 18 September 2018, ahead of the scheduled high-level UN General Assembly meeting due to take place on 26 September this year at the organisation’s headquarters in New York. The report will serve to provide a detailed perspective for all participating heads of state and various other officials. It is expected that around 50 heads of state will be in attendance. This is the first high-level gathering to be scheduled among global leaders, purely to discuss the TB crisis (2) and is entitled; ‘United to End Tuberculosis: An Urgent Global Response to a Global Epidemic.’
The underlying purpose is clear – there is an urgent need to accelerate efforts in the fight against TB. High-level commitments have been made; now with more clarity on the current status of the health concern, further efforts are necessary if disease incidence and its consequences are to be dramatically reduced.
Global commitments to end the epidemic status of TB
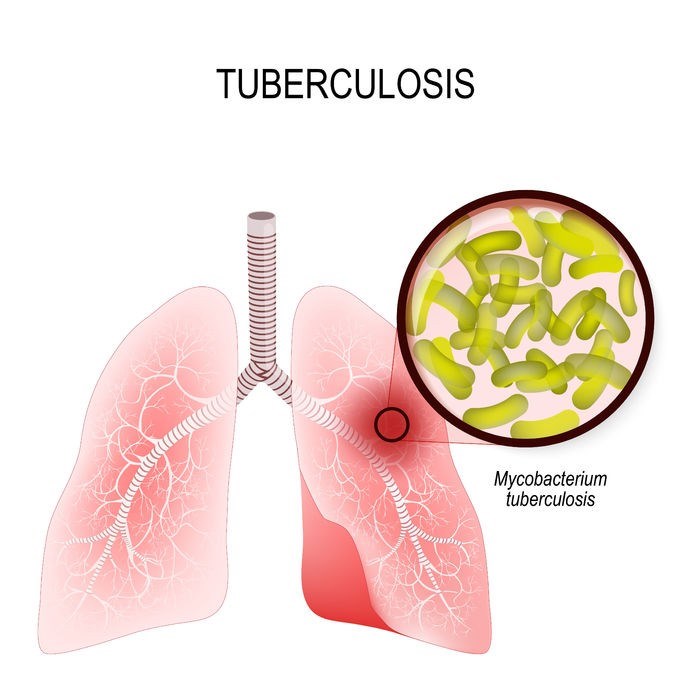
The first drug treatments for TB became available in the 1940s. For a long time, the public feared this infectious disease, believing that if you caught the infection, you were going to die. For many nations, the rate of infection and mortality has been high, creating a major health burden. In general, TB is still labelled as an ‘epidemic’. Why? It is a still a disease that affects millions around the world.
2030 – this is the year targets have been set for. The United Nations (UN) and WHO member states have a signed commitment to this date, all agreeing to do their part to end the global epidemic of TB. These commitments have been reinforced by various official strategy meetings including the ‘End TB Strategy’ held by the WHO at the World Health Assembly (May 2014) and the UN Sustainable Development Goals / SDGs (September 2015).
The targets, set in 2015 (as part of the SDG meeting), are to reduce TB fatality numbers by 90% and infection incidence by 80% by the year 2030. These are sizable yet decidedly achievable commitments. Afterall, preventative measures and improved treatment options are already in play and can effectively control the disease, and its ability to spread.
In November 2017, the WHO held the first ‘global ministerial conference’ in the Russian Federation, so as to strengthen the level of commitment made between the member states. More than 1 000 participants were present and included various state leaders and ministers of health from at least 120 countries. The Moscow Declaration to End TB was signed.
In May this year, commitments were further solidified at the World Health Assembly – All members agreed to accelerate their efforts in combatting the disease. This month’s UN General Assembly meeting will further stress this very point if the targets set are to be met.
A glimpse into Global Tuberculosis Report 2018 (3)
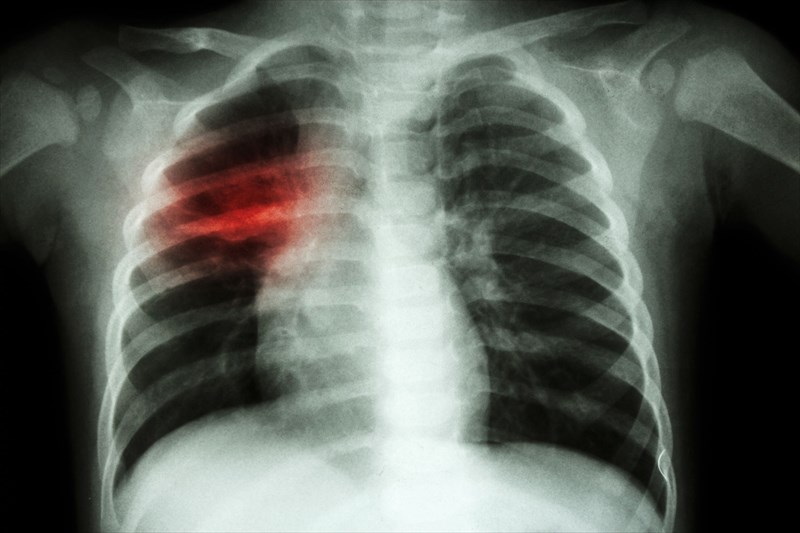
TB is among the top 10 causes of death in the world.
The WHO’s report is largely based on data acquired from the World Bank, UN agency databases and individual member countries. The annual reports provided help to give an overall status of the health concern, detailing the current disease statistics and the levels of progress made at regional, country and global levels.
Not only is TB a leading cause of death on a global scale, it is also the leading cause of fatality from a single infectious agent. The disease is still largely associated with HIV infections. Of the 1.6 million people who died from TB in 2017, 300 000 fatalities are attributed to those who were HIV-positive.
As many as 10 million new TB infections occurred worldwide in 2017.
Of these, a little more than half were adult males (around 5.8 million). Around 3.2 million adult females and 1 million children make up the remainder of this figure.
All of the UN member countries’ populations experienced new infections across various age groups. The WHO compiled a list of ’30 high TB burden countries’ which the report’s authors attributed around 87% of the world’s new cases to. These included the likes of India, China, the Philippines, Indonesia, Pakistan, Bangladesh, South Africa and Nigeria. The WHO European Region and the Region of the Americas each tallied around 3% of the world’s cases in 2017 respectively.
The report estimates that around 1.7 billion individuals may also likely have a latent TB infection (i.e. one that is asymptomatic / non-active) and are at risk of developing the full-blown active disease at some stage during their lifetime.
Globally, around 558 000 infections appeared to be resistant to first-line antibiotics.
One of the most effective medications used for TB treatment is rifampicin. The report highlights that a growing number of TB infections are now not only resistant to this antibiotic, but multiple drug therapies too. As many as 82% of rifampicin resistant infections in 2017, the report claims, are ‘multidrug-resistant (MDR-TB), which further adds to the woes of the growing global antimicrobial resistance crisis.
As at the end of 2017, multidrug-resistant infections in India tallied around 24%, followed by China at 13% and the Russian Federation at 10%. Of the TB multidrug-resistant incidence numbers, the report estimates that around 8.5% can be classed as ‘extensively drug-resistant’ (XDR-TB).
Progress is being made – TB fatality ratios have decreased from 23% (in 2000) to 16% (in 2017).
The report authors acknowledge that committed efforts to reduce TB as a disease burden is making some progress and seeing results. However, the pressure is still on to meet the 2030 targets. While most countries are achieving improvements, progress in this regard is marginal. On a global scale, the incidence of new infections is down to around an average 2% per year. The WHO does not regard this as good enough and believes that efforts to decrease the disease burden will need to be accelerated if targets will be met.
En route to the 2030 target, milestones along the way form part of the committed agreement, and WHO is ensuring that all member states keep this in mind.
The first milestone is set for 2020, under 2 years from now. At this stage, the agreement between the parties aims to achieve a global incidence reduction of at least 4 / 5% per year, and a fatality decline (case fatality ratio) of 10%. By 2025, the WHO would like this incidence rate reduced by at least 10% and the fatality ratio to around 6.5% per year.
Some countries or regions have made better progress than others so far in this regard – notably, between 2013 and 2017, the European Region achieved a 5% TB incidence reduction and the African Region, a 4% decline overall per year.
A boost in efforts within the African continent may indeed have a lot to do with the declines achieved. The region is also plagued by an HIV epidemic, and general disease care and prevention measures for both infectious diseases has been stepped up in recent years. The southern African region has seen between 4 and 8% reductions in TB within South Africa, Namibia, Lesotho, Zambia, eSwatini (formerly known as Swaziland) and Zimbabwe. A boost in efforts within the Russian Federation has also seen an average TB case reduction of around 5% during the same time period.
HIV-negative fatalities associated with TB have also improved over the years – the total estimation was 1.8 million in the year 2000. Based on the 2017 figure, this is a 29% reduction. HIV-positive associated fatalities were tallied at 534 000 in 2000. Based on the 2017 figure, this is a 44% improvement.
Overall HIV-associated deaths appear to be reducing at around 3% per year but there are still high disease burden rates within some of the WHO regions, namely the Russian Federation, Vietnam, Sierra Leone, Ethiopia and Kenya.
The report emphasises that thus far, improvements made in diagnostic and treatment processes have meant that around 54 million fatalities between the years 2000 and 2017 have been averted.
On the agenda at the UN General Assembly meeting
Incidence and fatality figures aside, there are several concerns to address if progress down the line can be adequately made…
Detection and treatment gaps…
The processes between notifying national authorities about new TB cases and reporting each and every one to the WHO requires improvement and consistency among member states. This, the report acknowledges may have an influence of the overall figures. Report authors have used the figures they have. Any unknown incidences are possible. Challenges in underdiagnosis due to a lack of sufficient healthcare access are part of this problem.
This is already an issue that has been recognised by the WHO – Together with Stop TB Partnership and the Global Fund to Fight AIDS, Tuberculosis and Malaria, the organisation launched the FIND. TREAT. ALL. (#EndTB) initiative (4). The initiative is geared towards assisting nations with accurate detection and treatment challenges and bridging the gaps that obscure the disease epidemic status figures.
Ensuring that all committed parties implement strategies that are in line with bridging these gaps, however they specifically apply within a specific region, will be a discussion point at the assembly meeting.
Implement urgent measures to circumvent drug-resistant TB and initiate better prevention…
Gaps in detection and treatment go hand-in-hand with challenges around drug-resistant infections. High numbers of new infections are having to be enrolled in second-line treatment regimens and the success rates are concerning.
The report highlights that overall, the global treatment success rate of this infectious disease stands at around 55%.
Drug susceptibility testing will need improved coverage too in order to help reduce instances of underdiagnosis, and by extension, assist with better overall care. Developments in new means of diagnosis and medications with improved efficacy and safety are also required.
Prevention measures are a key factor too. The report mentions the bacille Calmette-Guérin (BCG) vaccine as an important measure in the prevention of the disease, and especially so where high latent TB infection figures exist and young children, who are vulnerable to infection are concerned.
The WHO strongly recommends preventative treatment for individuals living with HIV and children under the age of 5, in particular (both of whom may have latent TB or may have been exposed to an individual with a confirmed case). Many who fall within these groupings may have access to the BCG vaccine, but are not receiving the preventative treatment measure. The report authors urge country leaders to ensure access to such care is encouraged within their populations.
This preventative treatment option should be highly effective. During 2017, 158 of the world’s countries had access to the BCG vaccine. An average 90% coverage rate was recorded within 120 of these countries. As a result, the WHO estimates that a minimum of 30 million individuals around the world should then have access to, and be eligible, for preventative treatment by 2022.
Boost funding contributions…
If any improvements are to be sufficiently made and challenges better overcome, an increase in funding (and a sustainable flow of contributions) is also likely to be addressed at this month’s meeting. As of this year, funding contributions have totalled around US$ 6.9 billion.
The WHO’s report estimates that a total of US$10.4 billion in funding is needed in order to meet the requirements of diagnostic and treatment services, as well as ensure the implementation of preventative measures. This figure is based on projected estimations during the years to come which could see the widening of gaps, causing a short-fall in being able to reach acceptable targets.
Points of discussion are likely to include from the source of this funding – the report mentions domestic sources within middle-income countries, public – private partnerships and international donors.
Research is a vital component when it comes to adequate funding. Although contributions have increased during the last several years, estimations for what is required is considerably less. During 2016, contributions for TB research peaked at US$ 724 million. The WHO estimates the current figure required to be around US$2 billion per year.
Research is necessary if the overall strategy targets set for 2030 are to be attained. The WHO recommends that technological breakthroughs with regard to research are needed by 2025 if the accelerated declines in TB incidences are to be met. Funding is thus critical.
Some of the priorities where research is concerned include improved developments where new medication treatments are concerned, as well as vaccines helping to reduce infection risk. Measures for rapid diagnosis and shorter and simpler treatment regimens are also key areas of focus for researchers.
Development in this regard has been slow and steady and could benefit from the boost additional financing could offer. At least 20 new medications, a handful of proposed treatment regimens and around 12 alternative vaccine candidates (still undergoing clinical trials) have filtered through the research pipeline.
Reinforce the commitment to achieve ‘Universal Health Coverage’
The authors of the report urge all committed parties to continue striving for UHC / Universal health coverage. Countries / regions must continue to address associated social and economic reasons for TB outbreaks wherever applicable. Such reasons include the likes of HIV infection and malnourishment (or extreme poverty), among others.
The ultimate goal is to ensure that all members of society, especially low-income populations, have access to and receive adequate healthcare. There is also a need to ensure that measures are in place to help prevent the incurred health expenses from becoming exorbitant financial burdens.
Nations must identify, and regularly monitor, applicable social and economic factors resulting in TB outbreaks within their regions and implement measures to counteract these underlying reasons that often drive disease occurrence.
It will also be requested that all nations ensure that adequate healthcare is available in order to prevent and treat TB, especially for those considered vulnerable to infection (high-risk populations).
Overall, the report makes it clear that the end of TB is not yet entirely foreseeable, and plenty more must be done to accelerate the progress of infection incidence reduction if ever the disease is to be rid of its ‘epidemic’ status.
The outcome of the upcoming high-level meeting will surely set further benchmarks for all parties to evaluate their levels of progress and reinforce commitments if the identified targets are to be met in the quest to eliminate TB in the years to come.
Promises are one thing, but action that influences the outcome on the scale required will be the true measure of success.
“We need to join forces to root out this disease that has a devastating social and economic impact on those who are “left behind”, whose human rights and dignity are limited, and who struggle to access care. The time for action is now,” says WHOs Global TB Programme Director, Dr Tereza Kasaeva.
References:
1. World Health Organization. 18 September 2018. Global tuberculosis report 2018: http://www.who.int/tb/publications/global_report/en/ [Accessed 20.09.2018]
2. World Health Organization. UN General Assembly High-level Meeting on Ending TB: http://www.who.int/tb/features_archive/UNGA_HLM_ending_TB/en/ [Accessed 20.09.2018]
3. World Health Organization. 18 September 2018. Global tuberculosis report 2018 - Executive Summary: http://www.who.int/tb/publications/global_report/Exec_summary_17Sept2018.pdf?ua=1 [Accessed 20.09.2018]
4. World Health Organization. Joint Initiative: "FIND. TREAT. ALL. #ENDTB": http://www.who.int/tb/joint-initiative/en/ [Accessed 20.09.2018]