
What is HIV?
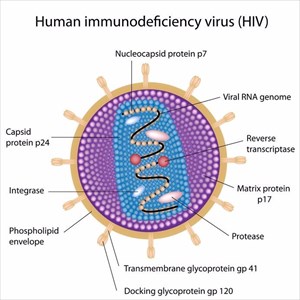
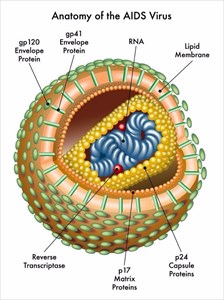
Normally the body’s immune system is able to fight off infection. The forceful nature of HIV means that the virus reduces the number of CD4 cells in the body, making an infected individual more vulnerable to a variety of other infections or other infection-related conditions, such as tuberculosis, candidiasis and cancer. The HIV virus uses proteins in the CD4 cells to produce a copy of itself, before destroying these cells.
This process is constant and can happen daily for as many as 10 years or more, even without the display of obvious symptoms. The constant battle within the body means that over time, it becomes more and more difficult for the body to protect itself and fend off illness. An infected person will constantly have their CD4 cell count monitored through treatment.
The virus is a life-long one with no cure and requires constant medical care and treatment in order to control it. Once infected, a person has a constant battle with a weakened immune system. The earlier an individual begins a treatment programme the better for their quality of life and ultimately, life expectancy.
One of the most important things regarding treatment with antiretroviral therapy (ART) is to prevent (or lower the risk of) further transmission (spreading of the virus), as well as to control the progression of the disease, prolonging the life of the infected person. If treatment is administered before the disease is too far advanced, a person’s life expectancy can be almost as long as someone without an infection.
The importance of testing can’t be stressed enough. It is the only way to determine the presence of the virus in the body. The process for testing is not nearly as complicated as you may think and can be requested at most medical clinics, hospitals, community health centres and even substance abuse programmes around the world.
What is AIDS?
If it happens, what this advanced stage effectively means is that the body’s immune system is so badly damaged that a person is at their most vulnerable for a variety of what is often termed, ‘opportunistic infections’. ‘Most vulnerable’ means that a person’s CD4 cell count has fallen below the 200 cells per cubic millimetre of blood mark (200 cells/mm3).
AIDS is classified as chronic and is considered potentially life-threatening. The life expectancy once this stage is reached can be anywhere between a year (without medical treatment) to 3 years (with medical treatment). Before the development of medical treatment, the advancement from HIV to AIDS could progressively occur within a handful of years. Now, if treatment is administered early enough following diagnosis, an HIV positive individual may never reach the most advanced stage of the virus.
Recent HIV/AIDS statistics
Upwards of 36.7 million people are currently living with HIV/AIDS across the world (as recorded at the end of 2015) according to UNAIDS (The Joint United Nations Programme on HIV/AIDS). Of these, an estimated 1.8 million infections are recorded in children. The vast numbers of infection mean that the disease is regarded as one of the world’s most serious health challenges.
Other facts include:
- During 2015, an estimated 2.1 million people across the world became newly infected with HIV, including at least 150 000 children.
- It is estimated that only 60% of those living with HIV have been tested and know their status. The remaining 40% are noted as having little access to testing services. The vast majority of these infections are those who reside in sub-Saharan Africa (low and middle-income countries).
- Across the world, an estimated 18.2 million who are living with HIV have access to ART.
- Since the start of the epidemic in the early 80s, an estimated 35 million individuals have died from HIV/AIDS related health conditions and illnesses. In 2015 alone, 1.1 million people were recorded to have died from HIV/AIDS related medical problems.
- Mother-to-child transmission of HIV has been notoriously high in low and middle-income countries. By the end of 2015, as much as 77% of infected pregnant women were provided access to ART medications which dramatically lowered the risk of transmission to their babies. Since 2010 mother-to-child transmission has declined by 50%, which marks significant progress in keeping new infections at bay.
Other Articles of Interest
Hepatitis
What is hepatitis? How does it affect the body? Should I worry? We look into everything you need to know about the effects of inflammation on the liver.

Shingles
Shingles is a viral infection, commonly known for its rash. it is the result of the chickenpox virus reawakening in your body, coming back as shingles. What happens to the body?

Pneumonia
What is pneumonia and how serious is it? Find out all you need to know about the condition here...
