| What is vaginal discharge? |
| Menopause and changes in vaginal discharge |
| Abnormal vaginal discharge |
| Causes of abnormal vaginal discharge |
| Diagnosing the underlying cause of abnormal vaginal discharge |
| Diagnostic tests for vaginal discharge |
| Treating vaginal discharge |
| Outlook |
What is vaginal discharge?
Vaginal discharge is a natural, healthy physiological function that is common daily occurrence in women of childbearing age and plays an important role in the female reproductive system.
The term 'vaginal discharge' refers to the clear or white fluid that is expelled from the vagina, often on a daily basis. This fluid / mucus is produced by vaginal and cervical glands under the influence of the female hormone oestrogen and assists the body in removing dead cells and bacteria from these areas, helping to keep the vagina clean, lubricated and infection free.
What is considered normal vaginal discharge?
Vaginal discharge differs from one woman to another, so what is normal for one may not always be normal for another.
Vaginal discharge often varies in1:
- Volume: 2 to 5ml per day is considered normal, however some women will produce more or less than others.
- Consistency: Normal vaginal discharge ranges from thin to thick and pasty depending on the time of a woman’s monthly cycle. The following are normal:
- Thick and white: This is generally experienced at the beginning of the menstrual cycle.
- Clear and watery: This can occur at various times of the cycle and may be heavier after exercise or when one is sexually aroused.
- Clear and stretchy: This type of discharge is indicative of ovulation and is usually experienced for a few days during this time, approximately 14 days after a menstrual period starts.
- Odour: Normal vaginal discharge is usually odourless but may have a faint (not bad) smell on occasion. The odour may be more pronounced if personal hygiene is compromised for some reason. Mild irritation, but not itching, of the vulva (i.e. skin around the vaginal opening) may also occur from time to time.
- Colour: While usually clear in colour, when exposed to air, milky white or yellow vaginal discharge may be observed.
- Brown vaginal discharge may be experienced following a menstrual period as old blood cells are removed from the cervix and vagina (old blood has a brown hue). Blood spotting or brown discharge may also occur mid-cycle during ovulation or in early pregnancy (this is referred to as implantation bleeding).
- Pink vaginal discharge is often experienced shortly after giving birth. This is due to the shedding of the uterine lining and is medically referred to as ‘lochia’.
As mentioned above, the variations in vaginal discharge are largely determined by hormonal fluctuations during the various stages of the menstrual cycle2. However, they may also be influenced by stress, pregnancy, hormonal birth control (i.e. pills, the patch, vaginal ring) or by taking certain medications.
Menopause and changes in vaginal discharge
Menopausal women generally experience less vaginal discharge than pre-menopausal women as well as increased vaginal dryness (i.e. a lack of lubrication) during sexual intercourse. In some instances, vaginal discharge, when present, may be very watery. These changes occur due to declining oestrogen levels and are considered normal during this stage of life. They can be addressed with medical intervention.
Abnormal vaginal discharge
While most vaginal discharge is completely normal and healthy, there are some instances where this is not the case. The following signs and symptoms are considered abnormal3:
- Yellow vaginal discharge: While discharge may naturally take on a yellowish tinge when exposed to air, a cloudy or strong yellow hue may be a sign of infection.
- Green vaginal discharge: This may be light green or yellowish-green in colour and may have a foamy texture. It can be indicative of an infection, particularly if it is thicker than normal, clumpy with a cottage cheese-like texture or has a foul odour.
- Blood-tinged or brown vaginal discharge: This type of vaginal discharge is considered abnormal when it is not obviously related to a menstrual period (i.e. occurring for a few days thereafter), early pregnancy or shortly after giving birth.
- White, yellow or grey discharge with a fishy smell: This may be caused by an infection.
- Thick, clumpy / cheesy texture: This may indicate an infection.
In addition, discharge that is accompanied by the following is abnormal:
- Itching: Particularly around the vaginal opening, vulva (external parts of the vagina) or labia (vaginal ‘lips’).
- Inflammation and pain: Redness, burning, swelling, tenderness or pain of vulval skin
- Rash or sores on the vulva or labia
- Foul odour
- Abdominal or pelvic pain
- Pain experienced during urination or sexual intercourse
If any of the above symptoms are experienced, seek medical help.
Causes of abnormal vaginal discharge
The lower female genital tract is home to 4. This ‘ecosystem’ can be thrown of balance by a number of internal and external factors5. This, in turn, can influence the texture, colour and odour of vaginal discharge.
The most common factors that cause changes in vaginal discharge include:
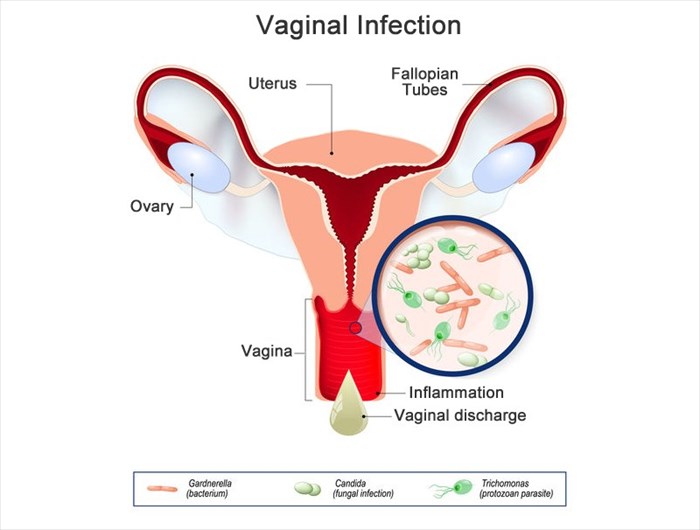
Infections
The most common vaginal infections (vaginitis) that cause abnormal vaginal discharge include2,6:
- Overgrowth of normal vaginal bacteria: Bacterial vaginosis (also referred to as BV or gardnerella) is the most common vaginal infection in women of reproductive age. It occurs due to an overgrowth of normal bacteria in the vagina, which upsets the natural flora balance. This type of infection causes vaginal inflammation, and while there are sometimes no evident symptoms, a clear, white or grey vaginal discharge with a ‘fishy’ smell7 may be experienced along with itching, redness, and swelling of the vagina and vulva. Bacterial vaginosis is not a sexually transmitted infection.
- Yeast infection: This is medically referred to as ‘vaginal candidiasis’ or ‘vulvovaginal candidiasis’ (VVC) and colloquially referred to as ‘candida’ or ‘thrush’. A vaginal yeast infection occurs when changes in the balance of bacteria and a naturally existing yeast (a type of fungus) called candida albicans occur. This upsets the natural balance of the vaginal flora and infection occurs, often causing itching around the vulva and vaginal opening, inflammation, pain and a thick, white, cottage-cheese consistency vaginal discharge. Typically, no odour is present. Thrush is common and can be transmitted between sexual partners.
- Trichomonas vaginalis (TV) / trichomoniasis / ‘trich’: This common sexually transmitted infection (STI) is caused by a microscopic parasite. The resultant infection can cause a frothy greenish-yellow discharge that is usually accompanied by a foul odour7, itching and pain during urination.
Other infections, conditions and disease that seldom cause vaginal discharge include:
- Chlamydia or Gonorrhoea / Gonorrhea: These sexually transmitted diseases (STDs) are often not detectable as they often do not cause symptoms. However, in some instances, cause a cloudy or yellow discharge which may be accompanied by other symptoms such as irregular bleeding between periods, pelvic pain and urinary incontinence.
- Desquamative inflammatory vaginitis (DIV): This non-infectious cause of inflammation of the vagina may cause a frothy, heavy vaginal discharge8 that may be yellow or greenish-yellow and occasionally grey in colour. It is usually accompanied by irritation of the vulva and pain during sexual intercourse.
- Atrophic vaginitis: This vaginal disorder occurs due to oestrogen deficiency. It is therefore most common after menopause due to declining oestrogen levels that result in the thinning, drying and inflammation of the vaginal walls. It can cause a yellow or greenish vaginal discharge and may be accompanied by mild redness and irritation, pain during sexual intercourse and an increased likelihood of vaginal trauma.
- Erosive lichen planus (ELP): This condition affects the mouth, oesophagus, anal and genital regions. The cause is unclear, but it has been linked to metabolic and immune disorders. It may result in a yellow or gray vaginal discharge that is accompanied by intense pain as well as pain during sexual intercourse and bleeding thereafter.
- Cervical or endometrial cancer: This can lead to a brown or bloody discharge that is not associated with the end of a menstrual period, implantation bleeding during early pregnancy or the shedding of the uterine lining after giving birth.
Infectious and disease-related causes of vaginal discharge will need to be evaluated and confirmed by a medical doctor in order for the appropriate treatment to be administered (more on this below).
Foreign bodies or substances
Vaginal discharge that differs from that which a woman usually experiences may be a result of the body’s reaction to a foreign body such as a:
- Condom
- Douche
- Forgotten tampon
Or a substance, such as:
- Antibiotics
- Hormonal birth control
- Steroids
- Scented / coloured soap or bubble bath
- Spermicides
These substances can change the pH (acidity) of the vagina, upsetting the delicate balance within its eco-system and leading to the overgrowth of yeast or bacteria that naturally occur in it.
In the above instances, with the exception of medication use (antibiotics, birth control and steroids), try removing the potentially offending substance/s and see if the condition clears up. If you feel a medication is to blame, discuss this with your doctor before discontinuing it.
Diagnosing the underlying cause of abnormal vaginal discharge
Can I diagnose and treat myself?
Many women would prefer to treat vaginal discharge themselves without consulting a doctor. While it may be tempting to do a Google search, self-diagnose (which will generally come out as thrush) and then purchase an over-the-counter cream, this could mean that the incorrect treatment is applied. While vaginal thrush (vulvovaginal candidiasis) is a common cause of vaginal discharge, it is not the only one. In fact, one study showed that only 11 percent of women accurately diagnosed their infection, and only 35 percent of those who had experienced a vaginal yeast infection previously self-diagnosed correctly9.
Making an incorrect self-diagnosis not only delays getting the correct diagnosis but can also lead to worsened symptoms and unnecessary costs. It is therefore advisable to not self-diagnose and attempt to treat vaginal discharge on your own using nothing but a search engine.
At home tests for vaginal discharge
In some countries, due to advancements in modern medicine, there are a number of at home tests that you can order online to help you to self-diagnose the underlying cause of your vaginal discharge. These include at home STD test kits, at home vaginal PH tests, as well as a vaginal discharge panel which tests for the 3 most common causes of vaginal discharge (Bacterial Vaginosis, Candida and Trichomonas). When ordered from reliable suppliers with laboratory analysis, and performed exactly according to the detailed instructions provided, these tests are often accurate and reliable.
Some of the underlying causes of vaginal discharge will require the prescription of antibiotics or scheduled ointments, and for this a doctor needs to be consulted.
Medical examination and diagnosis
There are a few things that you can do to assist a doctor in making an accurate diagnosis of the underlying cause of vaginal discharge:
- Refrain from self-treatment attempts as this can complicate things and make an accurate diagnosis more difficult.
- Note the dates of your last menstrual period as well as the dates of any irregular bleeding or spotting that may have occurred in addition to the changes in vaginal discharge experienced. Pay attention to its consistency (texture), colour and smell.
- Also note any other symptoms, if any, that you may be experiencing.
- Record any recent changes in the medications or health supplements you’ve been taking as these may be a contributing factor.
What to expect during a medical consultation?
An appointment with a general practitioner will usually be adequate to obtain a diagnosis of the underlying cause of irregular vaginal discharge. For your own comfort, try to schedule this at a time other than during your period and do not douche before your appointment.
As with any doctor’s appointment you will explain the reason for your visit, and a doctor may ask the following:
- Your age?
- The date of your last menstrual period?
- When did the abnormal discharge begin? What does it look and smell like?
- What symptoms are you experiencing in addition to the discharge?
- Are you experiencing any itching, pain or burning in the genital area?
- Do you have any back, abdominal or pelvic discomfort or pain?
- Have you recently used any tampons, pads, douches, lubricants or feminine hygiene products?
- Are you sexually active?
- Do you have a new sexual partner or more than one? This question is for no other reason but to determine your risk factors for potentially contracting a sexually transmitted infection (STI), which could cause abnormal discharge. This is nothing to be nervous or embarrassed about, sexually transmitted infections are exceptionally common these days and doctors treat them on a regular basis.
Next a physical examination will be conducted. This will involve:
- A pelvic exam: A physical examination of the outer parts of the genitals may be conducted. If a vaginal discharge is present it will be noticed right away. Your doctor will take note of its appearance (colour and consistency) as well as any odour present. He or she will also examine the genitals for signs of irritation, redness, swelling, sores or abnormalities that may be present. Based on these findings he/she may elect to perform an internal exam.
- Internal examination: To do this, the doctor will insert a speculum (a metal or plastic hinged device that looks like a duck’s bill) into the vaginal opening, this will then be opened to spread the vaginal walls so that the doctor can get a better look at the vagina and cervix. While this is not a comfortable exercise for all women, it should not be a painful procedure. Take a deep breath and try to relax as much as possible so as to relax the pelvic muscles.
- Obtaining a sample: During the pelvic examination a doctor may take a sample for testing using a thin cotton swab. If you haven’t had one recently, he/she may also conduct a Pap test to collect cells from the cervix. These samples will be used to test for infection.
Diagnostic tests for vaginal discharge

Laboratory testing to determine the underlying cause of vaginal discharge may involve one or more of the following:
- Vaginal pH testing: This test determines how acidic the vaginal environment is. Maintaining a healthy pH balance is essential for health. Normal vaginal pH is considered to be below 4.5 and levels generally range from 3.8 to 4.210. Infectious conditions like bacterial vaginosis and trichomoniasis increase pH and result in higher levels. This test often prompts further testing in the form of microscopy11.
- Microscopy:
- A test will be conducted wherein the collected sample will be examined under a microscope to determine the presence of trichomonas, yeast or clue cells (vaginal tissue cells with bacteria attached which signal a bacterial infection). The presence or lack of white blood cells (leukocytes) will also be noted. The presence of these in higher numbers shows that the body’s immune response is active and that the immune system may be fighting off an infection.
- Other microscopy tests can be done to check for fungi, confirm bacterial vaginosis and identify the specifics of the bacterial cells which will lead to a final diagnosis.
Treating abnormal vaginal discharge

The treatment of irregular vaginal discharge will be determined based on the underlying cause. A doctor may be able to make a diagnosis based on the examination or may recommend delaying treatment until the test results come back. Once the results are back it is important to understand what the underlying cause of the symptom is.
Treatments based on the underlying cause are generally as follows7,12:
Bacterial vaginosis (BV)
The most common treatment of this condition involves the administration of antibiotics, namely metronidazole and clindamycin. Both are available in pill and gel or cream form (metronidazole in pill form is marketed as Flagyl, while the cream form is marketed as metrogel).
Bacterial vaginosis can be treated in pregnant woman and a doctor will prescribe antibiotic medications accordingly.
It is important to note that treatment regimens do change and depend on the doctor's preferences. Be guided by your doctor and follow instructions as given. The treatment of sexual partners is not usually needed in a case of bacterial vaginosis.
Vulvovaginal Candidiasis (Vaginal yeast infection / vaginal thrush)
This type of infection may be classified as uncomplicated (in about 90% of cases) or complicated (10% of cases) based on certain criteria. Uncomplicated cases generally occur in healthy, non-pregnant women who experience mild to moderate symptoms as a result of infection with Candida albicans. These infections are typically experienced infrequently (less than 3 times per year).
Complicated cases involve far more severe symptoms, occur recurrently (more than 3 times per year), and are often due to infection with other candida species (particularly C. glabrata). Pregnant women, women with poorly managed diabetes or compromised immune systems are also classified as complicated cases.
Vaginal yeast infection treatment will depend on the classification made during a diagnosis.
Uncomplicated vaginal yeast infection treatment
There are two commonly prescribed forms of treatment:
- Vaginal cream / tablet / pessary: The treatment of vaginal thrush often involves the administration of a cream, tablet or pessary. These are applied or inserted into the vagina at night, before bed using an applicator. Both over-the-counter and prescription treatments are available, and your doctor will generally advise on which one to use based on the severity of the infection. Treatments may last one, three or seven days, but may vary depending on the severity of the infection present.
- Oral treatment – Yeast infections may also be treated with a prescription antifungal medication known as fluconazole (sold under the brand name Diflucan). A single dose (150mg tablet), taken by mouth (i.e. swallowed with water) is usually only necessary for those with uncomplicated infections and with the availability of generic forms of the drug, it is often more cost effective than antifungal creams. Side effects which include headaches, rash and stomach upset are generally mild. While interactions are rare at the dosage levels used to treat vaginal thrush, fluconazole does interact with a number of medications so it’s important to discuss all medications and/ or supplement you are taking with your doctor. This medication has also not been approved for use during pregnancy.
Both topical creams and oral medications are equally effective. Generally, symptoms resolve within a few days of commencing treatment. If vaginal discharge persists, book a follow-up consultation with your doctor.
Complicated vaginal yeast infection treatment
Women with persistent vaginal thrush symptoms will usually be prescribed an extended course (often 7 to 14 days) of treatment with an antifungal vaginal cream/tablet/pessary and/or a longer course of oral treatment. In severe resistant recurring cases a course of the oral medication can be given on a weekly basis for as long as 6 months if required. A mild corticosteroid cream may also be prescribed to help relieve symptoms until the antifungals take full effect.
It is possible to treat vaginal thrush in pregnancy and a doctor will make recommendations according to the severity of the infection present.
As vaginal thrush is rarely spread to sexual partners, it is generally not considered necessary to treat partners unless they show symptoms too.
Trichomoniasis
Vaginal discharge as a result of trichomoniasis is generally treated with oral antibiotics. While topical cream forms of these are available for application to the vagina, they are not as effective at treating trichomoniasis as the oral versions, which are therefore preferred.
Pregnant & breastfeeding women with trichomoniasis
Treating a trichomoniasis infection in pregnant women is often recommended as it can increase the risk of preterm birth and babies being smaller than their gestational age14.
Metronidazole (Flagyl), one of the most commonly prescribed antibiotics to treat this condition, is secreted in breastmilk. This means that a breastfeeding infant will be exposed to the medication, although in lower doses than would be used to treat an infected infant. Nevertheless, some doctors may recommend pre-pumping breastmilk to be used for between 12 and 24 hours following a single dose of the medication so as to minimise infant exposure.
Testing partners with trichomoniasis
Trichomoniasis infections do require the treatment of sexual partners in order to ensure that they do not recur. It is also necessary to re-test all infected women and their partners at a follow-up visit.
Chlamydia
Chlamydia infections are generally treated with oral antibiotics.
**MyMed Memo: It is especially important to treat pregnant women with chlamydia to prevent the infection from passing from the woman to her infant in the birth canal.
It is also necessary for sexual partners to also be treated.
Gonorrhea / Gonorrhoea
In uncomplicated urogenital gonorrhea infections, dual antibiotic therapy is recommended in the form of one intramuscular injection and oral medication.
Infected pregnant women will receive treatment for this infection.
It is also necessary for sexual partners to also be treated if a Gonorrhoeal infection is present.
Desquamative inflammatory vaginitis (DIV)
Desquamative inflammatory vaginitis is usually treated with either antibiotics or glucocorticoids which are powerful anti-inflammatory medications14 . Both are usually administered intravaginally using an applicator.
It is important to note that relapse after treatment ends is relatively common. So, if symptoms resurface, a follow-up visit to your doctor may be required.
It is not necessary to treat a sexual partner for this type of infection.
Atrophic vaginitis
Due to the fact that atrophic vaginitis (also referred to as vulvovaginal and urogenital atrophy) occurs due to a lack of natural oestrogens in the body15. Hormone replacement therapy (HRT) is usually the most effective treatment for the entire condition. Low-dose vaginal oestrogen therapy generally clears the vaginal discharge experienced as a result of this condition.
Preparations of vaginal oestrogen treatments include those in the form of vaginal tablets or capsules, vaginal rings or creams.
Erosive lichen planus (ELP)
While women affected by vulvar lichen planus can experience periods of remission with treatment, there is no cure for this condition. First-line therapy generally involves the administration of a potent topical corticosteroid ointment which acts as an anti-inflammatory.
Ointment is usually applied to the area involved for an extended period of time (often two to three months). A follow-up evaluation will then be required to determine whether maintenance therapy should begin or if an alternative medication is required.
Cervical or endometrial cancer
In cases where vaginal discharge is caused by cervical or endometrial cancer, treatment will be designed according to the type and stage of cancer present.
Outlook
Due to the fact that abnormal vaginal discharge is the result of one of a few underlying conditions, once the cause has been identified and treated, this symptom usually resolves. In some cases, depending on the cause, vaginal discharge may recur and require follow-up treatment. It is, however, important to be able to distinguish between a normal and abnormal vaginal discharge and if there is any uncertainty a medical opinion should be obtained.
References
1. Spence D, Melville C. Vaginal discharge. BMJ. 2007;335(7630):1147-1151. doi:10.1136/bmj.39378.633287.80
2. Rice A, ElWerdany M, Hadoura E, Mahmood T. Vaginal discharge. Obstetrics, Gynaecology & Reproductive Medicine. 2016;26(11):317-323. doi:10.1016/j.ogrm.2016.08.002
3. Vaginal Discharge | Female Health Topics for Teens. Pamf.org. http://www.pamf.org/teen/health/femalehealth/discharge.html. Published 2013. Accessed April 2, 2019.
4. Hickey R, Zhou X, Pierson J, Ravel J, Forney L. Understanding vaginal microbiome complexity from an ecological perspective. Translational Research. 2012;160(4):267-282. doi:10.1016/j.trsl.2012.02.008
5. Farage M, Miller K, Sobel J. Dynamics of the Vaginal Ecosystem—Hormonal Influences. Infectious Diseases: Research and Treatment. 2010;3:IDRT.S3903 .doi:10.4137/idrt.s3903
6. Spence D, Melville C. Vaginal discharge. BMJ. 2007;335(7630):1147-1151. doi:10.1136/bmj.39378.633287.80
7. Hainer B, Gibson M. Vaginitis: Diagnosis and Treatment. Am Fam Physician. 2011;83(7)(Apr 1, 2011 Issue):807-815. https://www.aafp.org/afp/2011/0401/p807.html. Accessed April 2, 2019.
8. Paavonen J. Desquamative Inflammatory Vaginitis. Infect Dis Obstet Gynecol. 1996;4(5):257-257.doi:10.1155/s106474499600049x
9. Ferris D, Nyirjesy P, Sobel J, Soper D, Pavletic A, Litaker M. Over-the-Counter Antifungal Drug Misuse Associated With Patient-Diagnosed Vulvovaginal Candidiasis. Obstetrics & Gynecology. 2002;99(3):419-425. https://www.ncbi.nlm.nih.gov/pubmed/11864668
10. Walker H, Hall W, Hurst J. Clinical Methods: The History, Physical, And Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990:Chapter 179.
11. Pavletic A, Hawes S, Geske J, Bringe K, Polack S. Experience With Routine Vaginal pH Testing in a Family Practice Setting. Infect Dis Obstet Gynecol. 2004;12(2):63-68. doi:10.1080/10647440400009839
12. Sobel J. UpToDate. Uptodate.com. https://www.uptodate.com/contents/bacterial-vaginosis-treatment. Published 2019. Accessed April 2, 2019.Silver B, Guy R, Kaldor J, Jamil M, Rumbold A. Trichomonas vaginalis as a Cause of Perinatal Morbidity. Sex Transm Dis. 2014;41(6):369-376.doi:10.1097/olq.0000000000000134
13. van der Velden V. Glucocorticoids: mechanisms of action and anti-inflammatory potential in asthma. Mediators Inflamm. 1998;7(4):229-237. doi:10.1080/09629359890910
14. Gandhi J, Chen A, Dagur G et al. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol. 2016;215(6):704-711.doi:10.1016/j.ajog.2016.07.045
15. Simpson R, Murphy R, Bratton D et al. Systemic therapy for vulval Erosive Lichen Planus (the ‘hELP’ trial): study protocol for a randomised controlled trial. Trials. 2016;17(1).doi:10.1186/s13063-015-1133-z