Is snoring serious?
It’s loud and harsh – there’s no mistaking the rumblings of a snoring person. A person who frequently snores may also develop a dry mouth or sore throat and feel like they are getting a cold or fighting allergies when instead, irritation to the tissues of the upper airway and resulting inflammation is being caused by vibrations due to snoring as well as dryness of the throat due to mouth breathing.
Simple snoring is not considered a life-threatening problem, but heavy, frequent snoring should be evaluated by a medical professional. While simple snoring may affect those try to sleep in the vicinity of a snorer and cause disrupted sleep, it can also deprive a person of getting enough rest themselves.
In short, snoring contributes to all-round fatigue. While unpleasant for those involved, mild snoring (with fewer heath risk factors) is unlikely to result in a serious health condition.
In some instances, a physical structure abnormality can result in snoring, at other times snoring may be indicative of an underlying health problem, and it is therefore wise to have chronic snoring that habitually disrupts the snorer’s sleep leaving them feeling fatigued, emotional and unable to concentrate medically assessed. A thorough assessment will either diagnose or rule out a cause. For the most part, snoring is reasonably manageable… even more so when a cause can be determined.
It’s merely about finding what works best to lessen the frequency and turn down the volume. If seeking a medical assessment, a consultation with an ear, nose and throat (ENT) specialist is a good place to start.
Is snoring a sign of obstructive sleep apnoea?
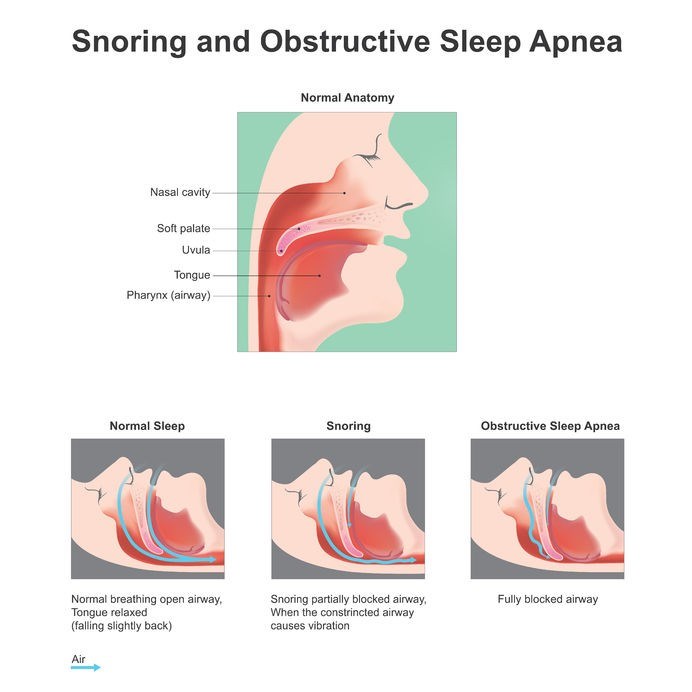
Snoring is a symptom of obstructive sleep apnoea but is not necessarily a classified sleep disorder in and of itself. While snoring is regarded as a sleep-related breathing problem, not everyone with a snoring habit has a serious medical condition. Simple snoring is more often just a nuisance for anyone exposed to it.
Frequent and loud snoring, however, can be indicative of a more serious health concern, like obstructive sleep apnoea (OSA) which occurs when the upper airways experience reduced airflow repeatedly during sleep. Breathing may become slow or temporarily stop altogether and will usually be accompanied by frequent awakenings whereby a person will experience gasps for air (a sudden choking or gulping reaction due to reduced or absent breathing capacity).
OSA events may occur as little as 5 times an hour, or as many as 30 (or more) times in an hour while asleep.
- A mild case of OSA is likely to be diagnosed should a person experience 5 to 14 apnoea episodes every hour.
- Moderate OSA will be diagnosed for apnoea episodes totalling between 15 and 29 every hour.
- Severe OSA will be diagnosed if person experiences 30 or more apnoea episodes every hour during sleep. (9)
Common symptoms of sleep apnoea include:
- Fatigue and excessive sleepiness during the day
- Problems with attention, concentration, as well as difficulties with verbal and visuospatial memory, and motor skills
- Headaches (commonly experienced upon waking in the mornings)
- Dry mouth
- Frequent awakenings during the night (often to urinate)
Women suffering from sleep apnoea tend to experience more frequent headaches, insomnia or sleep deprivation, as well as anxiety and depression. Children with the condition may experience hyperactivity and bedwetting, as well as problems with their academic performance.
Common causes of OSA include underlying medical conditions or an abnormality in a person’s physical structure – causes can thus range from large tonsils, excess weight gain or obesity, endocrine disorders (hypothyroidism, polycystic ovary syndrome / PCOS and acromegaly), certain genetic syndromes (affecting the structures of the face or skull, like a cleft lip or cleft palate or Down syndrome), neuromuscular disorders, or even failures of the heart or kidneys (this is experienced in the advanced stages of these diseases due to an accumulation of fluid in the neck).
Undiagnosed, OSA can lead to the development of more severe complications and thus must be appropriately evaluated by a medical doctor for treatment. Undiagnosed or untreated for extended periods of time, OSA can cause inflammation in the body which results in reduced blood oxygen levels. This drop in oxygen triggers a ‘fight or flight’ response in the body which then elevates blood pressure and heart rate, forcing a person to awaken from their slumber so that the upper airways can open and normal breathing be restored.
If left untreated, the cycles of increased and decreased blood oxygen levels as a result of OSA can contribute to more serious and inflammatory complications like atherosclerosis (plaque accumulation in the blood vessels), which can then place a person at higher risk of having a stroke or heart attack. Chronic inflammation that develops in the body can also result in injury to the pancreas, placing a person at risk of developing type 2 diabetes.
Aside from the more serious implications of OSA, other adverse effects can include:
- Regular problems with concentration
- Frequent outbursts of anger or frustration
- Behavioural troubles (especially in children with the condition)
- Restlessness during sleep
- A sore throat (often experienced first thing in the morning)
- Sleep deprivation can also result in an increased risk for motor vehicle accidents
When to consult a doctor
Simple snoring that is particularly loud and frequent and does not appear to respond to efforts to lessen its occurrence can be assessed by a medical doctor. If a snorer notices any other adverse effects or changes in their health, a medical assessment is recommended to either rule out or diagnose a potential underlying cause.
If any of the most common OSA signs and symptoms are frequently experienced, it is best to seek a medical evaluation as soon as possible, especially if sleep patterns are disrupted by breathing pauses during sleep (these are often more easily identified by a bed partner than the sufferer themselves) and regular awakenings where gasping (sometimes expressed as a very loud snort) are experienced.
Among the signs and symptoms of OSA, snoring is likely to be one of the top few that prompt a medical evaluation. A bed partner is sometimes a better gauge for assessing the occurrence and frequency of snoring should clarity need to be provided.
A doctor will make their assessment of any underlying snoring cause/s by conducting a full medical review (including a personal and family history of sleep associated troubles). Questions may be asked so as to assess just how much of an impact a sufferer’s snoring is having on their overall sleep quality, and where relevant, capacity to function optimally during the day.
Some of these questions may include:
- Do you snore / have you been made aware that you snore most nights of the week (more than 3 times a week)?
- Is your snoring / have you been made aware that your snoring is loud (i.e. can your snoring be heard in an adjacent room)?
For those with suspected OSA, questions may involve:
- Have you noticed that you gasp for breath during sleep or has a bed partner made aware that you stop breathing while asleep?
- Do you find that you fall asleep during the day or doze off when you are idle, not active, or even sitting in traffic?
- Are you being treated for high blood pressure (hypertension)?
A doctor may ask for an indication as to how long / regularly a person has been snoring, as well as whether or not a person has experienced any recent weight gain or stopped exercising frequently.
Recent air travel may also be a factor – low-oxygen environments are known to worsen OSA-like symptoms for a short period of time following air travel. Diagnosed OSA patients are typically cautioned against high altitude air travel without supplemented oxygen (in addition to CPAP / continuous positive airway pressure treatment). (10)
A full list of medication and supplement use will also be requested. From there, a physical examination will be conducted, and a series of tests (including blood tests) may be recommended to either diagnose or rule out underlying conditions. Sleep studies (either within a sleep centre or at home) will help to determine apnoea events and their severity, as well as monitor key areas of concern, such as blood oxygen levels, and brain, muscle and heart activity during sleep.
Both simple snoring or snoring as a symptom of a sleep disorder such as OSA, can be effectively managed. For more serious sleep disorders, oral device / appliance therapies (breathing devices, like CPAP and mouth pieces) and surgery (involving implants which assist with delivering mild stimulation to muscles in order to assist in opening the airways during sleep, or a nerve stimulator which helps with the positioning of the tongue) are available options. More on these here.
References:
9. National Heart, Lung and Blood Institute. Sleep Apnea: https://www.nhlbi.nih.gov/health-topics/sleep-apnea [Accessed 21.02.2018]
10. Centers for Disease Control and Prevention. June 2017. Altitude Illness. Chapter 2 - The Pre-travel Consultation: https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/altitude-illness [Accessed 21.02.2018]