What is bronchitis?
At the turn of a new season it’s not uncommon for the body’s immune system to weaken, causing a dreaded cold or flu (influenza).
Generally, a cold or flu heals within a few weeks. With a weakened immune system, sometimes the body doesn’t return to normal and a respiratory infection develops.
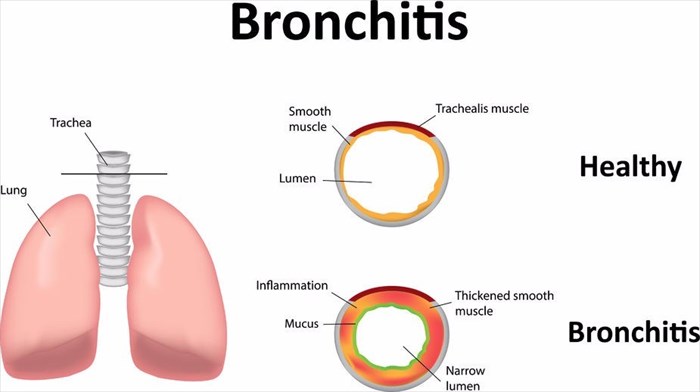
Bronchitis is a lower respiratory tract condition that occurs when the lining of the bronchial tubes becomes infected. A build-up of mucus (sputum), which is often discoloured, and a persistent cough then develop.
How does bronchitis develop?
A viral condition, bronchitis generally develops from the same organism that causes colds and flu. Sometimes bronchitis can develop as a result of a bacterial infection.
As the body naturally fights off germs, bronchitis develops when the bronchial tubes become inflamed, swell up, and begin to produce a build-up of mucus. This then results in narrow openings for air to travel to and from the lungs, making it more difficult to breathe.
Types of Bronchitis
There are two types of bronchitis:
- Acute bronchitis: This is the most common variation of bronchitis with symptoms lasting for several days, but coughing may last for a few weeks, even after the patient has been treated for acute bronchitis.
- Chronic bronchitis: A more serious condition whereby inflammation of the bronchial tube lining is constantly irritated. This type repeatedly comes back or doesn’t tend to clear up at all. Usually experienced by smokers, this bronchitis type can develop from chronic obstructive pulmonary disease (COPD), a long-term lung disease that occurs when air sacs in the lungs thin out. COPD may also be called Emphysema.
Other Articles of Interest

Fever (Temperatures)
Often a sign that something is wrong in the body, a fever is a typical symptom of a variety of different illnesses. When should you worry about having a fever?

X-rays
X-rays are a very common procedure that many of us have had to have or may have in the future. If you want to know more about the imaging test, read all about it here.

Pneumonia
What is pneumonia and how serious is it? Find out all you need to know here...