How are bunions treated?
Options for the treatment of bunions involve non-surgical (conservative) and surgical methods.
1. Non-surgical treatment options
Conservative treatment does not typically involve reversing the developed deformity, but is targeted more at alleviating symptoms and reducing the risk of further distortion.
Options and recommendations will involve:
- Shoes that fit: The wearing of orthopaedic shoes with customised inserts or soles (custom insole orthotics which are often padded) and uppers and arch supports, which also provide sufficient wiggle room for toes and encourage a more normal shape. Customisation is important as it can help to avoid placing unwanted pressure elsewhere on the foot which can lead to worsened symptoms or the development of further complications. A doctor will also encourage certain types or styles of footwear that will provide better comfort – i.e. discourage the wearing of heels, or encourage supportive activewear shoes (like running shoes with supportive soles and wide toe boxes) for walking, as well as sandals or shoes made of soft leather.
- Pressure relief: Pressure can also be reduced by having a doctor tape or pad an affected foot – this helps to correct foot structure and encourage a ‘normal position’ (alignment). Splints can also be customised for comfort (often worn at night to hold a big toe in a straighter position).
- Medications: The taking of recommended over-the-counter analgesics such as acetaminophen, NSAIDs (nonsteroidal anti-inflammatories) pain relievers (ibuprofen, acetaminophen, aspirin or naproxen), as well as others to relieve swelling or inflammation.
- Cortisone injections (at controlled doses) are another option a doctor may recommend for the relief of pain caused by inflammation (and specifically where discomfort is caused by an inflamed bursa). The potential risk of side-effects will be weighed against the benefits of relieving significant pain.
- Antibiotic therapy: This may be required if constant pressure or friction has caused a breakdown of the skin and thus, infection, of the foot.
- Compresses for pain and swelling relief: Pain and swelling can be alleviated with heat pads or compresses or regular warm foot baths. Cold compresses and ice packs can also help to alleviate swelling in the foot.
- Activity adjustment: A doctor may recommend limiting or avoiding activities which aggravate symptoms, such as certain sports or even standing for long periods of time.
- General health: A doctor may also suggest care when it comes to overall health, specifically with regards to weight, should fluctuations appear to be problematic. A heavier weight can place more pressure on the feet and joints, thus worsening a bunion and its uncomfortable symptoms.
2. Surgical treatment options
Opting for surgical intervention to treat a bunion is a serious consideration which a doctor is not likely to encourage purely for cosmetic reasons. In severe instances, a person’s quality of life and ability to live normally on a day-to-day basis is considerably compromised, and in these cases surgery may be recommended.
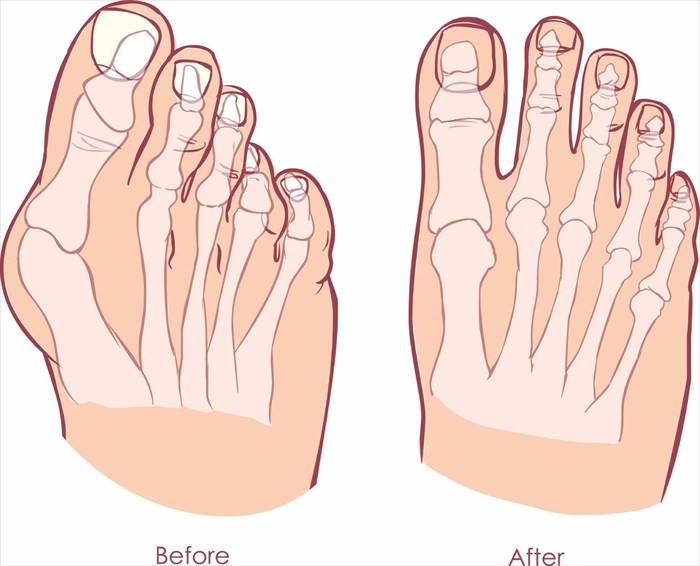
Surgery can help to restore a big toe to its most natural (straight) position, but cannot promise to eradicate all symptoms associated with a bunion’s development. Recovery post-op is also something to take very seriously and requires the patient to stay off their affected foot for at least 4 to 12 weeks (depending on the surgical technique used). A complete recovery can take up to one year.
There are a variety of specialised procedures performed for bunions, with all of these generally aiming to restore as much normal function as possible by removing the bony protuberance, and realigning the joint, tendons, ligaments and nerves in the toe. In so doing, pain and inflammation which could not be alleviated sufficiently enough through conservative measures alone, can be significantly reduced.
A surgeon will assess whether a person is a candidate for surgery by taking X-rays and measurements in order to classify a bunion (i.e. identifying its severity level – mild, moderate, or severe). This helps determine the type of surgical techniques that will likely achieve the best outcome. The more severe the bunion, the more complicated a surgical procedure may be.
Overall health assessments including the strength of bones and connective tissues will also be assessed. A surgeon will also note other factors for candidate consideration such as a person’s age, and general activity level.
Surgical options in relation to categorised severity (2) include:
- Mild bunion: A surgeon will make a small incision in the toe, exposing the area of bone / joint that will be worked with. The technique most often used for mild deformations is known as a bunionectomy. This involves the shaving off of an enlarged bone (bony excess) on the outside of the metatarsal head (outer top portion of the toe joint), as well as the realignment of the muscles, ligaments and tendons surrounding the joint. Swollen tissue at the joint may also sometimes be removed. The recovery period for this surgical procedure is normally between 3 and 4 weeks. A full recovery can sometimes take up to 8 weeks. A surgeon will request that a postoperative shoe be worn during recovery (this will be customised for the patient). The surgery may not entirely correct a bunion deformity, but can alleviate painful symptoms considerably.
- Moderate bunion: The procedure for a slightly more pronounced bunion is similar to that of a bunionectomy, but involves an osteotomy technique (the cutting, not shaving, and repositioning of the metatarsal head). A surgeon will cut bone close to the metatarsal head in order to shift it into its previous (normal) position, better aligning the joint / bone (thus straightening it as far as possible). Pins, wires, screws or even a plate are then used to secure the bone, holding it in its adjusted position. Tendons or ligaments may also be made longer or shorter. The recovery period for this surgical procedure is normally around 4 to 6 weeks. A patient will be fitted with a short cast, and given crutches for movement without placing pressure on the foot during the recovery period.
- Severe bunion: For severe deformity, a surgeon will cut away bony excess at the metatarsal bone head (as is done for a moderate bunion), and at the base of the metatarsal joint, removing the wedge-like bone structure and realigning the metatarsal (by rotating the bone), and securing it with pins and screws. Muscles, tendons and ligaments will also be corrected and realigned in the process. Should a joint be so severely deformed that it is beyond repair, an artificial joint may be inserted to replace it during the procedure. Recovery can take between 6 and 12 weeks, and also involves the wearing of a cast and use of crutches.
Note: Osteotomy techniques vary according to the surgeons who developed them and are thus so named – Akin / Mitchell / Ludloff / Wilson osteotomy etc.
Bunionectomy and osteotomy surgical techniques are performed under local (the foot is numbed, and a patient is lightly sedated / relaxed), general (medication is given to place a patient in a state of sleep) or spinal anaesthetic (a medication injected into the spine will numb the entire area below the waist), and will take place in a hospital or surgical centre. The procedure is typically done on an outpatient basis (i.e. a person can return home on the same day once deemed fit for discharge).
Surgical risks which will all be considered before a specialist will elect to proceed with surgery include:
- Potentially adverse reactions to anaesthetic (allergic reactions, problems with breathing, infection, bleeding and the formation of blood clots).
- The recurrence of a bunion formation (this is a common complication for those who previously underwent a bunionectomy which involves the shaving of the bony prominence and not a correction of the underlying deformity).
- Under or over correction of the joint (i.e. the surgery may not be successful).
- The cut bone portions reuniting too slowly or not joining together at all during the healing process (this is referred to as non-union and may require an additional surgery).
- Irritation occurring as a result of the pins, screws, wires or plate used to hold the bone / joint together – this can lead to stiffness and excessive scarring.
- The fact that surgery does not alleviate the symptoms associated with pain.
- Decreased flexibility or movement of the big toe – often due to the bone shifting back to its previously deviated position before the surgery (i.e. a patient may thus not be able to move their toes as easily as they could before the surgery).
- The development of numbness (or nerve damage), stiffness or arthritis in the big toe
Before a surgical procedure (usually a week or two beforehand):
- Medications that interfere with blood clotting (blood thinners) will need to be discontinued (i.e. aspirin, naproxen and ibuprofen).
- Cease smoking habits (as this can interfere with wound or bone healing)
- Ensure that a surgeon is well aware of all other medications and supplements being taken (including herbal / natural varieties), pre-existing medical conditions (such as heart disease or diabetes), or whether an illness has been experienced shortly beforehand (such as a bout of flu or the common cold, or even a herpes infection).
- On the day of the procedure, a patient should follow all recommended instructions a surgeon has given (including those involving eating and drinking).
After a surgical procedure
Once a surgeon is happy with the initial post-op recovery (the first hour or two after surgery), a patient will be discharged (usually on the same day if no worrisome complications occur). Homecare recommendations may likely involve the following:
- Taking care of swelling: Post-op swelling is normal. A surgeon will recommend keeping the leg of the affected foot elevated on 1 or 2 pillows or cushions (placed just beneath the calf muscle or foot) when at rest (sitting or lying down). This will help to reduce swelling considerably in the days and weeks following surgery. It can take between 9 and 12 months for swelling to reduce fully following a surgery.
- Caring for the incision wound: The incision in the skin that was made to access the bone / joint will have been stitched up and covered with a sterile dressing. A surgeon will request that this be kept clean and dry until it is time for it to be removed. He or she may recommend taking a sponge bath, while keeping the foot covered so as to avoid contact with water. A post-op follow-up consultation will also be scheduled to monitor healing.
- Pain management: A surgeon will prescribe medications to be taken during recovery to help with managing pain. Dosage instructions (including duration) will be recommended, as well as some other anti-inflammatory drugs which can be bought over-the-counter (as needed). Medications prescribed will take into consideration any others required to be taken for the treatment of an existing condition, or those which are known to trigger an adverse reaction. The toe joint may be a little stiff for a few weeks or month post-op as well.
- Activity considerations: Depending on the type of surgical procedure, a surgeon will advise that a patient remains immobile (off the foot) for a period of time. Different surgical techniques (used according to the severity of the bunion) require specific recovery durations in order for the patient to heal appropriately. A surgical shoe or cast may be required to be worn for up to 8 weeks in order to maintain the appropriate position during healing. Movement during the recovery period won’t necessarily be outright forbidden (it is important to move following a surgery so as to avoid the development of blood clots, and complications such as deep vein thrombosis). Walking aids, such as crutches may be provided, but a walker or Zimmer frame can also help with keeping maximum pressure off the healing foot during periods of movement. Walking only short distances is recommended, especially during the initial 2 or 3 weeks following surgery. The surgeon is also likely to recommend muscle strengthening exercises to help with maintaining a range of motion in the foot and ankle.
- Shoes: When it comes time that shoes may be worn again (usually at around 3 months post-op), a surgeon will recommend those made of soft leather, athletic shoes, as well as any other style which has plenty of room in the toe box portion. He/she will also strongly advise against narrow styles and heels.
If the following occurs post-op, an appointment with the surgeon should be made as soon as possible:
- Fever or body chills develop
- The skin around the incision wound becomes warm and red (inflamed)
- The incision wound begins to bleed or leak fluid
- Pain does not subside even while taking medications to alleviate it
- Pain, swelling and redness develops in the calf muscle
Outlook for bunion surgery
In order for a positive outlook to be achieved, it is important that expectations are accurately discussed between the surgeon and patient beforehand. While surgery does involve a cosmetic change, it is not primarily aimed at achieving this. Surgery is mostly considered for cases of severe or debilitating symptoms, and aims to restore as much normal structure and function as possible. It cannot guarantee a total deformity reconstruction or a “perfect-looking foot”. The reality is that a big toe may never be completely straight again.
A surgeon will also set expectations for those who favour narrow shoe styles – these may likely never be worn again. The recovery period also needs to be made very clear before electing to have bunion surgery. Recovery takes a considerable amount of time and will impact a person’s day-to-day lifestyle for a few weeks to several months (at the very least).
If all goes well, once healed, a person should experience less pain following surgery, and be able to walk comfortably, as well as wear shoes with a little more ease.
Adopting conservative treatment measures going forward can also help considerably in keeping new bunion formations and associated symptoms at bay. High on the list is shoe care considerations and adjustments. The more pressure that can be taken off the MTP joint, the better for overall foot mechanics.
If a bunion is left untreated, what can go wrong?
Leaving a bunion well alone will not make it go away. Once developed, bunions become a permanent fixture. Deformity will progressively take place over time, and other complications can occur too.
These include:
- Bursitis: Inflammation of the bursae (small fluid-filled sacs / pads which primarily cushion the joint / bone, tendons and muscles. This results in considerable pain and limited movement.
- Hammertoe: The middle joint of a toe begins to bend abnormally due to increased pressure, causing pain.
- Metatarsalgia: Pain and inflammation which develops in the ball of the foot.
- Other ailments: Further deformity of the foot or toes, persistent stiffness in the toes, and chronic pain in the toes and or entire foot.
Reference:
2. Harvard Health Publishing - Harvard Medical School. June 2011. What to do about bunions: https://www.health.harvard.edu/diseases-and-conditions/what-to-do-about-bunions [Accessed 03.11.2017]