Dandruff: Causal associations
The actual cause for the characteristic formation and desquamative (flake shedding) pattern of dandruff is seemingly still up for debate. The normal physiological spectrum of scaling does not yet appear to be very well understood in relation to the formation of dandruff. More research is sure to surface in the years to come to determine a precise cause, and thereby help to identify more effective treatment measures, with the ultimate goal being a cure. For now, causes may be multifactorial and depend on various aspects pertaining to individual conditions.
There are some predisposing factors or associated links that have been researched thus far as potential causes of dandruff.
These include the likes of:
- Possible similarities relating to causal influences between dandruff and seborrheic dermatitis (SD).
- Individual susceptibility which involves the composition of dandruff formation and stratum corneum (epidermal barrier) dysfunction, as well as immune responses, stress and genetic factors.
- Fungal colonisation and the potential role of malassezia fungi in dandruff and SD formation.
- Bacterial associations with dandruff formation and the possibility that the presence of bacteria may have more of a causal influence than fungi.
- Non-microbial associations with dandruff - i.e. causes not related to microorganisms like bacteria.
1. Dandruff and seborrheic dermatitis (SD)
SD is known to be more chronic in nature (with frequent relapses), ranging from mild dandruff (physiological scaling) to more severe, widespread dermatitis (inflammation of the body’s skin and / or scalp). The exact cause of SD, like dandruff, is unknown but also appears to have multifactorial influences.
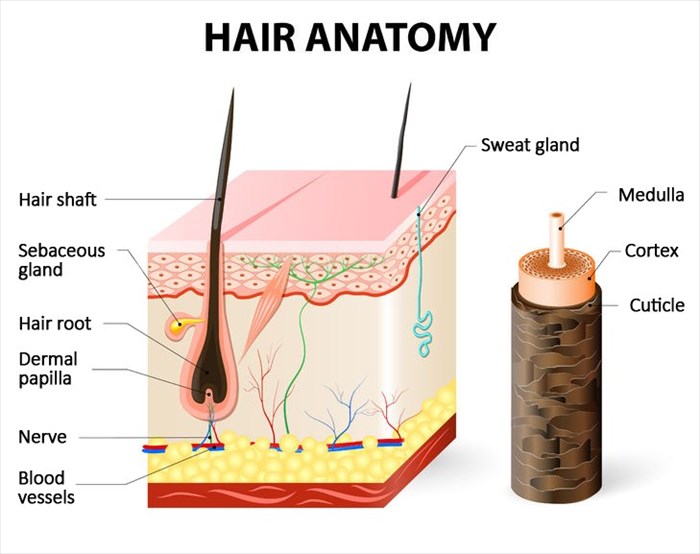
SD most commonly affects the sebaceous areas of the skin (exocrine glands which naturally secrete the oily or waxy substance, sebum, as a means to lubricate or waterproof hair and skin). Thus, the most commonly affected areas of the body associated with SD include the scalp, face (eyelids, eyebrows, creases of the nose and lips), the outer parts of the ears and chest / torso.
Scales may be oily or greasy as a result of their location in areas of the body where excess oil secretion occurs and as such, cause sticky dandruff. Itching and erythema (superficial reddening of the affected area) may worsen if an infection occurs. As a papulosquamous disorder, SD can also present as papules (small pimple-like swellings under the skin) along with scales / flakes on the affected areas of skin.
Many individuals affected by SD are generally in good health (i.e. they do not appear to have any other medical illnesses as possible underlying causes of the condition). Some associations have, however, been made with other conditions, particularly HIV (human immunodeficiency virus) infections and AIDS (acquired immunodeficiency syndrome) and neurological disorders like Parkinson’s disease (this condition leads to increased perspiration which may exacerbate SD), as well as individuals with central nervous system disorders. Exactly why individuals with these conditions appear to be more severely affected by SD is not entirely clear as yet, although increased sebum production is fairly common amongst these individuals and as such, is believed to play a distinctive role.
Aside from excessive oil gland activity, SD is also associated with yeast organisms like malassezia, genetic factors and changes in a person’s skin barrier function. This is also true for dandruff.
Symptoms of SD can be further aggravated by:
- Changes in seasons and humidity level (the condition is often worse during the winter months which are cold and dry).
- Emotional stress and trauma to the affected areas (including the scratching of itching skin) – this is also true for mild dandruff conditions.
SD that affects the scalp of infants is common during a baby’s first year of life and often referred to as ‘cradle cap’ (infantile seborrheic dermatitis). It is generally characterised by thick, crusty white or yellow scales on the scalp although cradle cap can also affect a baby’s facial area (eyebrows, eyelids and creases of the nose), as well as the back of the neck, ears, armpits or groin. A small amount of oozing drainage or crusting can sometimes occur, as well as erythema (superficial redness) or bleeding (due to the infant scratching the scaly areas).
It is thought that cradle cap occurs due to the stimulation and growth of a baby’s sebaceous glands. Factors which play a role in stimulating this growth involve the adrenal glands (androgen production and the enlargement of neonatal adrenal glands) and the transplacental transfer of androgens from the mother during birth. Like dandruff and SD, cradle cap isn’t contagious nor is it an indication of poor hygiene practices.
Like SD (including cradle cap), dandruff is considered sebaceous in nature, but not in an inflammatory capacity, and only affects the scalp. Neither condition is considered to be a disease of the sebaceous glands. As mentioned above, the production of excess sebum does, however, play a role in its development, since the areas of the body with the most or largest sebaceous glands are most typically affected.
The severity spectrum of SD ranges from mild (dandruff) to exfoliative erythroderma (exfoliative dermatitis).
Many consider dandruff and SD to be the the same basic condition of the scalp, only really differing in physiological magnitude (or degree of severity). Dandruff is considered to merely be a milder form of the condition with minimal (or subclinical) inflammation (if any at all).
2. Individual susceptibility
The composition of dandruff and skin barrier dysfunction
The normal physiological spectrum of dandruff scaling (i.e. the replenishment process of skin cells) is thought to play a role in the composition of skin cell flakes. Dandruff composition and its various influencing factors form part of a rather complex and interwoven process of events.
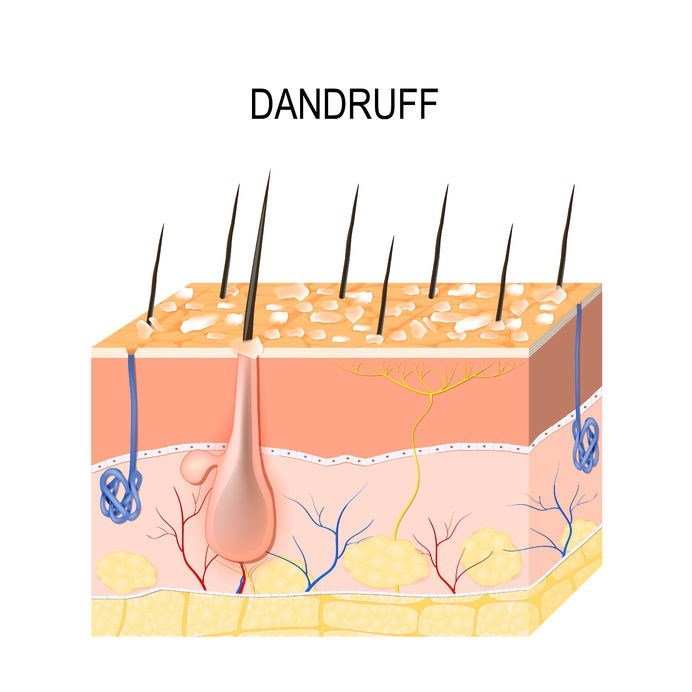
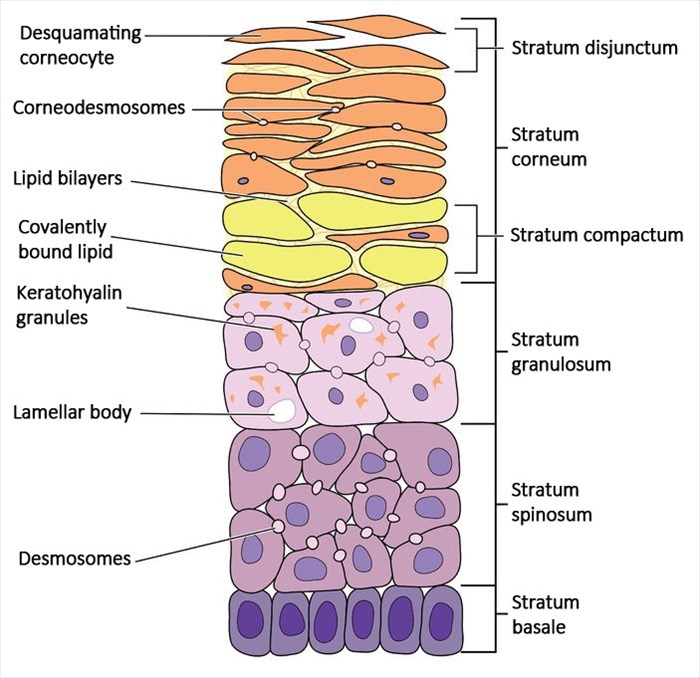
Essentially a cluster of corneocytes (squames - thin flakes / scales), dandruff flakes / scales display an increased degree of cohesion to the surface of the scalp (or stratum corneum – the outermost skin layer that consists of keratinised skin cells / dead skin cells filled with keratin proteins) from which they ultimately detach (shed).
The excessive production of new skin cells (hyperproliferation and altered corneocyte maturation) meant to replace old and dead ones on the surface of the scalp leads to parakeratosis, a process whereby the keratinisation of cells occurs in the outermost skin layer (stratum corneum) while retaining cell nuclei. This then leads to an abnormal replacement process involving squames with nucleated cells – meaning that skin cells which reproduce themselves by dividing occur in larger numbers than they should during the normal replenishment process.
Parakeratotic cells form part of the composition of dandruff. The size and distribution of flakes / scales differs from one person to the next. The prevalence of dandruff from one area of the scalp to another may also differ with each shedding occurrence that results in flaking of the scalp.
In individuals susceptible to dandruff, skin barrier dysfunction also plays a role. The stratum corneum is multi-layered, consisting of flattened and anucleate (cells without a nucleus) corneocytes that are surrounded by multiple fine sheets (or flakes) of lipids. The primary composition of lipids includes ceramides, cholesterol and fatty acids.
This structure serves as a protective barrier for the body and scalp, maintaining hydration in the skin and preventing water loss. It is also an effective protective mechanism against toxic materials, irritants and harmful microorganisms which can result in ill health. As a protective barrier, its thickness typically remains constant as a result of the continuous renewal process. However, the natural renewal process changes during dandruff formation, compromising the integrity of the scalp and this may have a causal impact in susceptible individuals.
The volume of barrier lipids in the scalp (i.e. a diverse group of compounds which include hormones, fats and oils) is reduced when a person is affected by dandruff and this compromises the level of protection offered. Trans-epidermal water loss (TEWL – a loss of water which passes from the inside of the body and through the epidermis / skin, evaporating from the skin’s surface) is commonly noted in those with dandruff of the scalp as the skin’s ability to retain adequate amounts of moisture is compromised. This, along with hyperproliferation and altered corneocyte maturation results in the subclinical nature of inflammatory response associated with dandruff.
Loss of water to the scalp also upsets the healthy function of the stratum corneum, causing an imbalance in hydration and flexibility.
Intercellular proteins, known as corneodesmosomes, latch together neighbouring corneocytes in the stratum corneum layer. Several classes of hydrolytic enzymes work with these proteins to facilitate the normal, healthy desquamation (i.e. shedding / skin turnover) process. In healthy skin, this helps to maintain skin integrity and health as well as thickness.
The surface of the skin must be well hydrated in order to facilitate normal desquamation. When corneodesmosomal hydrolysis is impaired, pathological skin disorders, like dandruff or seborrheic dermatitis occur. Increased sebum production also disrupts the desquamation process and the normal functionality of lipids.
Colder temperatures and low humidity levels are associated with aggravating dandruff. Seasonal changes impact the barrier lipid levels, thus making dandruff worse during the colder winter months of the year.
Psychological or emotional stress causes increases in circulatory stress hormones and thus impacts the epidermal permeability barrier (i.e. the skin’s barrier to water loss) and its ability to recover and replenish sufficiently. This too worsens dandruff. Such skin barrier dysfunction can induce scalp dryness, itching and irritation, along with the formation of characteristic dandruff flakes / scales.
Predisposing genetic factors and stress
There may be inheritance patterns in individuals prone to developing dandruff or seborrheic dermatitis. Like other causal associations, this area is also limited in terms of conclusive research findings but is regarded as something that may potentially play a role. Some inheritable factors which form part of ongoing research involve the following:
- Enlarged sebaceous glands
- Hyperkeratosis (an abnormally thickened outer layer of skin)
- Acanthosis (also involving a thickening of the skin)
- Parakeratosis (an incomplete maturation of epidermal keratinocytes which causes the abnormal retention of nuclei in the stratum corneum)
- Myelin Protein Zero-Like 3 (Mpzl3 transmembrane protein) skin abnormalities (may cause disruption in the regulation of epidermal differentiation and dandruff / SD flakes or scales)
Sebum changes and elevations in hormones are associated with potential underlying influences (like stress) in certain people who may be more susceptible to dandruff or SD. Sebum changes have been noted in individuals with Parkinson’s disease suggesting possible neuro-endocrinological influences specifically with regard to elevations in α-melanocyte stimulating hormone (α-MSH).
Stress (psychological or emotional) is also a potentially aggravating factor impacting the body’s natural defence mechanisms (immune system) by causing them to weaken, making a person more vulnerable to, for instance, colonisation by naturally occurring microbial organisms (like malassezia – discussed below).
3. Dandruff and fungal colonisation
Malassezia (a genus of fungi also known as Pityrosporum ovale) has been identified as an underlying cause of dandruff for many years, potentially producing the abnormal physiological reaction that results in inflammatory symptoms.
It is believed that the growth of this fungi is closely associated with the activity of the scalp’s sebaceous glands. Melassezia is lipid-dependant (i.e. it is a lipophilic yeast) but it is yet to be conclusively implicated in the formation of dandruff and seborrheic dermatitis as researched associations have only produced limited causal findings to date.
This skin saprophytic species (an organism which feeds on dead organic material) colonises the skin (i.e. is present on the skin) of healthy individuals. It naturally occurs on the skin of most but has been seen to grow / proliferate in individuals with excess sebum production (sebum triglycerides) by up to 75% (7). An increased number of organisms (yeast) as a result, is what is believed to contribute to the inflammatory responses observed in individuals with seborrheic dermatitis in particular. Why this has an influence on dandruff and SD conditions is not entirely clear.
Studies do not appear to have been able to definitively demonstrate whether symptoms of dandruff or SD occur as a result of an immune response to malassezia or its by-products which are comprised of free fatty acids or lipases (i.e. enzymes which activate the hydrolysis of fats, a chemical breakdown as a result of a reaction with water). This is because some individuals do not display clinically immunologic abnormalities (i.e. there may be an inflammatory response present, but local inflammation of the scalp may not always be visible). Inflammatory reactions experienced may not be as a result of immune responses either, but rather as a reaction to the irritant (i.e. the release of lipases / inflammatory free fatty acids such as oleic and arachidonic acid produced by malassezia).
The number of organisms present does not seem to correlate with the severity of seborrheic dermatitis or dandruff (i.e. a higher number of organisms on the scalp does not mean that dandruff or SD increases in severity). Normal levels of malassezia species have been seen in individuals with dandruff and SD, sometimes even in those exhibiting an abnormal immune response.
Certain species of malassezia, like Malassezia globosa and Malassezia restricta, have been noted more often in those affected by dandruff and seborrheic dermatitis than in unaffected individuals. These species appear to be more dominant on the scalp than in other areas of the body which are sebum-rich.
Other species which are active in those with dandruff problems include:
- Malassezia furfur
- Malassezia obtuse
- Malassezia pachydermatis
- Malassezia sloofiae
- Malassezia sympodialis
Therapeutic agents with antifungal properties have shown some degree of positive treatment results in some individuals (and are thus currently the favoured first-line treatment options) even though the precise mechanisms for potential fungal involvement are not very well understood at this stage.
A fungal infection with malassezia species may or may not be a causal factor in the development of dandruff. Malassezia may be associated with T-cell depression (the suppression of white blood cells which normally assist with adapting the body’s immune response to the presence of pathogens) and elevated sebum levels. Fungal colonisation may also contribute to the development of parakeratosis and stratum corneum barrier dysfunction. Further research is needed to determine direct links demonstrating just how malassezia contributes to the characteristic hyperproliferation and flaking formation, and inflammatory responses noted in individuals with dandruff and seborrheic dermatitis, as well as its relationship with epidermal skin barrier defects.
For now, it may be agreeable for many that malassezia may not be a direct cause of these flaking scalp conditions but rather an associated predisposing factor along with individual susceptibility. The exact mechanism of this fungus as it relates to a cause remains relatively obscure for the time being and continues to be researched.
4. Bacterial associations with dandruff formation
More recent research has associated dandruff related conditions with bacterial infections as possible underlying causes rather than fungal colonisation and infection. It has been determined that bacteria species that exist on the scalp include the likes of Propionibacterium (anaerobic bacteria) and Staphylococcus (aerobic bacteria), which appear to occur in more predominant populations than any malassezia species or other bacterium present. Thus, bacteria could possibly have a stronger causal relationship in the development of dandruff than fungi. (8)
Aerobic bacteria can grow and survive in an oxygenated environment while anaerobic bacteria do not require oxygen in order to grow.
Increases in sebum secretion and high-water content may provide a favourable habitat for bacteria as well as fungi. Sebum feeds both bacteria and fungi which can co-exist, enabling the species that are present on the scalp to grow and thrive. Propionibacterium can secrete free fatty acids onto the skin and produce proteins (bacteriocins), promoting bacterial adherence. The secretion of these proteins can suppress the growth of the more aerobic bacteria. Staphylococcus bacteria appears to inhibit any overgrowth of Propionibacterium. This then results in reductions in Propionibacterium and increases in Staphylococcus, which, unlike fungal causes, could have an influence on the severity of dandruff in affected scalps.
Treatment which shifts the balance the opposite way (decreasing the amounts of Staphylococcus bacteria in relation to Propionibacterium) could thus help to ease the severity of dandruff. This, coupled with better regulation of a person’s natural physiological processes (i.e. the renewal and shedding skin cell cycles), is thus hypothesised to potentially prevent the development of dandruff.
Further research is required, taking into consideration physiological or anatomical differences (including perspiration, sebum and hormonal production) relating to the different age groups and genders.
5. Non-microbial associations with dandruff
- Flaking / scaling (desquamation of the scalp): This may be influenced by excessive sunlight exposure.
- Scalp irritation: This may be caused by excessive shampooing of the hair, over combing or brushing and sensitivities to certain cosmetic products, dirt or contact with dust.
Further research could better help to understand these associations and determine just how much of an impact they have on the development of dandruff conditions.
References:
7. How to Overcome Dandruff and Other Scalp Disorders. March 2013. Dandruff - An Overview: https://books.google.co.za/books?id=CLdMCAAAQBAJ&pg=PT3&dq=dandruff&hl=#v=onepage&q=dandruff&f=false [Accessed 12.03.2018]
8. US National Library of Medicine National Institutes of Health. May 2016. Dandruff is associated with the conjoined interactions between host and microorganisms: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4864613/ [Accessed 12.03.2018]