When to see a doctor about gastritis-related symptoms
Stomach irritation or inflammation and indigestion affects nearly everyone at some point in their lifetime. In most cases, mild indigestion symptoms are short-lived and don’t require medical care or intervention.
If signs and symptoms occur for at least of a week or longer, the inflammation being experienced could indicate gastritis and should be diagnosed by a medical professional.
Red flags include:
- Stomach discomfort that occurs after taking over-the-counter or prescription medications
- Vomiting of blood
- The presence of blood in stools (faeces)
- Stools that appear black and tarry.
If you are concerned about anything you are experiencing or have any of the above red flag symptoms, it is recommended that you seek medical advice and / or assistance from your general healthcare provider (GP).
You can prepare for your appointment by ensuring in advance that you avoid any potential dietary (foods that are spicy, fried, acidic or fatty as well as alcohol) or medicinal triggers. It will also help to bring along a list of all medications and supplements you are taking, or even questions you feel strongly about asking your doctor. Key personal information such as major stresses or recent life changes are also worth mentioning during your appointment.
How is gastritis diagnosed?
Your doctor will review your personal information (including family history) and likely ask you the following kinds of questions during your consultation:
- What are your symptoms?
- How long ago did your symptoms begin and have they been constant or occasional?
- Would you describe any pain as mildly uncomfortable or burning?
- Have you noted anything, such as eating certain foods, that seems to worsen your symptoms?
- Have you recently lost any weight?
- How often do you drink alcohol (and how much) or take pain relievers such as aspirin, ibuprofen or naproxen?
- How would you rate your levels of stress?
- Have you ever experienced or treated ulcers before?
Your doctor is then likely to perform a physical exam, and if gastritis is suspected, he or she will treat you accordingly. In cases of recurrent gastritis, your doctor may refer you to a specialist in digestive disorders (gastroenterologist) for further examination, possible diagnosis and a treatment plan.
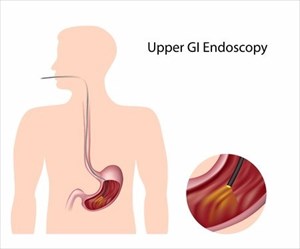
- An upper endoscopy: An endoscope (a long thin tube containing a tiny camera lens at the tip) is inserted through the mouth and down through the oesophagus (throat) into the stomach. This tiny camera will assist your doctor in assessing the condition of your stomach lining and whether there is any inflammation. A small sample (or biopsy) of the stomach lining may be taken during this process if anything unusual is noted, and sent for analysis in a laboratory. A biopsy can also detect the presence of H. pylori bacteria in the stomach lining.
- Blood tests: Various blood tests may be performed, depending on what your doctor deems necessary. He or she may want to have your red blood cell count tested to determine whether or not you have anaemia (not enough red blood cells). Your doctor may also wish to screen you for the presence of infections (such as Helicobacter pylori) or pernicious anaemia (a type of vitamin B-12 anaemia).
- Stool test (faecal occult blood test): A possible red flag of gastritis is the presence of blood in the stool. As such, your doctor may request a sample to check this. Helicobacter pylori can also be detected in a stool test (and even a breath test).
- Breath test: Your doctor will ask you to drink a small glass of clear, tasteless liquid containing radioactive labelled urea. You will then be asked to blow into a bag, which is sealed.If your breath sample contains the radioactive carbon dioxide which is released after the bacteria has broken down the urea in the stomach, you will have a Helicobacter pylori bacterial infection.
- X-rays (barium swallow): You may be given a barium solution (barium sulphate) to swallow before an X-ray if your doctor would like to check for anything unusual happening in your upper digestive system. The solution enables your doctor to look at clear images taken of your oesophagus, stomach and small intestine, and see if there are any abnormalities or areas of concern. The clear / white metallic liquid coats the digestive tract and makes any abnormalities, such as ulcers, more visible on X-rays.
