Something to take into consideration when choosing a birth control method is your overall health.
Factors relating to your health may put you at risk (whether in a mild or serious capacity) for experiencing problems.
Some birth control methods may merely just not be safe for you. If in doubt, consult your doctor to help you assess levels of safety. Your doctor will likely want to know the following in order to assist you as some health issues may limit your choices:
- Do you smoke?
- Are you pregnant?
- Is there a possibility you could be pregnant?
- Are you breastfeeding?
- Do you have other serious health conditions, such as heart disease, high blood pressure, headaches and migraines or diabetes?
- Have you ever had deep vein thrombosis (blood clots in the legs)?
- Have you ever had other blood clot disorders in the lungs, such as pulmonary embolism?
- Do you have a close family member who has had blood clots in the legs or lungs?
- Have you been diagnosed with and treated for breast cancer?
- Have you had a sexually transmitted infection, such as gonorrhoea?
Birth control side effects
- IUDs: Insertion can be painful for some women. Other women may experience heavier menstrual periods (or more irregular ones) and more discomfort with cramps. These types of side effects often go away within the first 6 months of use. Risk of an infection is highest when the IUD is inserted. It is not a recommended birth control method for women who may have or who have had an STI, might be pregnant, have untreated cervical cancer, uterine cancer, or who experience unexplained vaginal bleeding. The copper IUD isn’t recommended for women who are allergic to copper or who have Wilson’s disease (a rare genetic condition that causes copper poisoning in the body). Other risk factors include women who have severe liver disease, and those who have or have had breast cancer.
- Intrauterine Ball (IUB): A woman may experience spotting, and / or longer and heavier menstrual periods following insertion of the device (i.e. changes in bleeding patterns). This can happen for at least 2 to 3 months following insertion but does typically resolve thereafter. On occasion, some women may experience short / mild fainting spells. Uterine perforation risk is low but can sometimes occur during insertion and placement. Although the risk is low, the device may fall out of place or be expelled (partially or completely falling out of the uterus). If a woman experiences pelvic pain, genital sores, unusual vaginal discharge (such as severe or prolonged bleeding), a missed menstrual period or unexplained fever, a consultation with her doctor should be booked as soon as possible for a thorough evaluation. If a woman and /or her partner experience pain during intercourse, or have been exposed to a sexually transmitted disease, a check-up is also required as soon as possible.
- Implant: An implant can sometimes move or migrate from the initial site of implantation (usually in the upper arm, right under the skin), making it difficult for your medical professional to find and remove (after a maximum of 3 years).
- Sterilisation: Men may opt for a vasectomy as a more permanent solution for birth control. A reversal is possible in some circumstances, but is a more complicated procedure (making it not always possible to reverse). Short term risk include swelling, bruising, bleeding inside the scrotum, presence of blood in the semen, and infection. Long term complications can lead to fluid build-up in the testicle/s and chronic pain. Women can opt for 2 different types of sterilisation: surgical (called tubal ligation) and non-surgical. Tubal ligation prevents pregnancy immediately after the procedure. Non-surgical sterilisation may take up to 3 months to be effective. Some tubal ligations may be reversible, but this is not often successful. A non-surgical sterilisation is not reversible at all. Non-surgical sterilisation is not an option for women who only have one fallopian tube, have had one or both fallopian tubes closed or obstructed or are allergic to contrast dye used in X-rays. Possible risks and complications can include infection and bleeding. Where a doctor is using inserts for sterilisation, there is a risk of the implant becoming dislodged or damaged in the uterus. Some women have experienced long-term chronic pelvic pain. In both male and female sterilisation procedures, although rare, tubes may heal after sterilisation. If this happens, pregnancy may occur. More often than not, however, this pregnancy will be ectopic (the foetus implants in the fallopian tube instead of the uterus). This can be life-threatening.
- Injection: If used correctly, the risk of pregnancy can be reduced in most women to as little as 1%. Common side effects include headaches, abdominal pain, dizziness, nervousness, decreased sex drive, weight gain, acne, stomach bloating, hot flushes, insomnia, achy joints, nausea, sore breasts, hair loss, depression, and decreased bone density. Although rare, more serious side effects can occur and will require immediate medical attention. These instances include major depression, pus or pain near the injection site (arm or buttocks), unusual or prolonged vaginal bleeding, yellowing of your skin or the whites of your eyes caused by bile flow problems, breast lumps, or migraines with aura (a blight, flashing sensation that precedes migraine pain).
- Patch: Less than 1% of women who correctly use the patch fall pregnant. When things do go wrong, as can happen with any hormonal form of birth control, the following side effects may be experienced: deep vein thrombosis, stroke, heart attack, pulmonary embolism.
- Vaginal ring: There is a slight risk of blood clotting, which can also occur with the use of birth control pills or patches (due to additional hormones in the body). With this comes an increased risk of deep vein thrombosis, stroke, pulmonary embolism and heart attack. Women who fall into a high-risk category (and for whom an oestrogen containing contraception will not be recommended) are those who smoke and are older than 35 years of age.
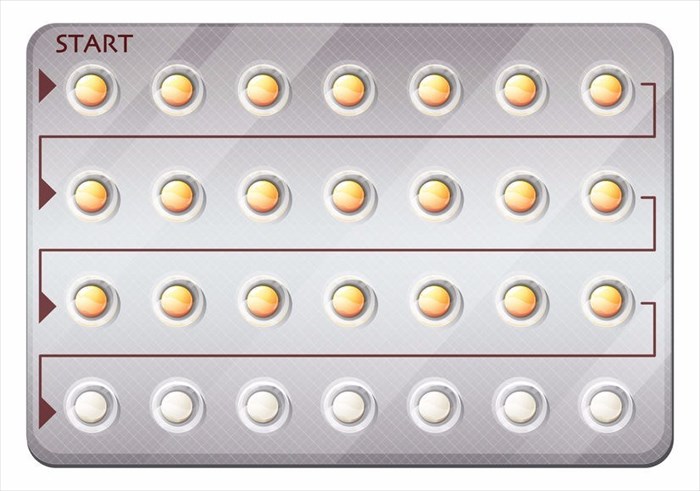
- Birth control pills (oral contraceptives): Every woman reacts differently to hormones, with many experiencing unpleasant side effects. Side effects that may stabilise or even go away within a few months can include decreased sex drive, nausea, spotting (or bleeding between menstrual periods), and breast tenderness. More serious side effects and complications include heart attack, stroke, deep vein thrombosis and pulmonary embolism. Women who are most at risk for developing blood clots are overweight, have high blood pressure, smoke and are on bed rest for long periods of time.
- Condoms: Male and female condoms can cause skin irritation (contact dermatitis) due to allergy or latex sensitivity (in this case you can opt for other varieties made from polyurethane or polyisoprene). A man or a woman can also experience dryness, discomfort or allergic reactions to spermicides, lubricants, scents and other chemicals used in condoms. Female condoms can be bothersome and uncomfortable to insert or wear during sex.
- Cervical barriers: Side effects are rare but can include urinary tract infections, vaginal irritation or allergic reactions to spermicide. Cervical caps are easy to use incorrectly, and can also slide or be pushed out of place during intercourse. Many women (and men) find them uncomfortable as well.
- Vaginal sponge: A sponge can break, especially when trying to remove it. If this happens and you can’t get all of the pieces out, you need to see our doctor as soon as possible to avoid an infection. If you are allergic to sulphites (a chemical often found in wine or food), you should not use this method of birth control or the spermicide that it is used with. Some are at an increased risk of toxic shock syndrome (TSS) which causes symptoms of fever, shock and organ damage.
- Emergency contraceptive pill: It is possible to experience side effects with ‘the morning after’ contraception option. These can include nausea, abdominal pain, unexpected bleeding or spotting, fatigue, headaches, dizziness, vomiting and breast tenderness.