Are there different IVF treatment techniques?
Assisting conception outside of the body does open up several avenues for different techniques which can be used in the process. It is a good idea to discuss all available options and their possible success rates with a fertility specialist before going ahead with the treatment to ensure that you (and your partner if applicable), as well as your doctor embark on the road most likely to produce the desired result (a healthy pregnancy).
Different techniques may benefit different individuals for a variety of different reasons. Your specialist will discuss in detail which could best work for you before going ahead with the treatment procedure.
IVF technique options for procedure consideration can include:
- Natural cycle IVF: This technique involves the harvesting and fertilisation of one egg that is released during a woman’s normal monthly menstrual cycle without the use of fertility medications (stimulating ovulation). The egg is then fertilised with donated sperm (either from an anonymous or known donor) in an attempt to produce a viable embryo for implantation. The risk of ovarian hyperstimulation syndrome (OHSS) is reduced, which can cause adverse symptoms of swollen and painful ovaries, abdominal pain, nausea and vomiting, diarrhoea, sudden weight gain, or severe problems such as shortness of breath or blood clots in the legs. OHSS occurs when fluid accumulates in the abdomen and pelvis, which may lead to blood clots. This method is also sometimes favourable in certain cultures and amongst religious groups who may dislike the idea of multiple fertilised embryos being created and going unused (these are either frozen or disposed of). Success rates of this technique are, however, not tremendously high.
- Mild stimulation IVF (or low dose IVF): Medications may be prescribed at a lower dose to stimulate ovulation or alternatively, they are given for a shorter period of time. Mild stimulation also reduces the risk of ovarian hyperstimulation syndrome, especially for those diagnosed with PCOS and trying to conceive. This technique is also effective in reducing menopause-like symptoms associated with stimulating ovulation with the standard medication dosage, which is physically more comfortable for a woman to experience. Mild stimulation, although more cost effective, however, doesn’t produce too many viable eggs for harvesting, which means that specialists are likely to have fewer embryos to work with for implantation. That said, the time between treatment cycles is also shorter, meaning that a woman can repeat IVF attempts more times (3 to 4) within a 6-month period than standard procedures (provided all attempts involve mild stimulation). And the difference in success rates, between standard IVF stimulation and mild stimulation, is minimal (almost the same).
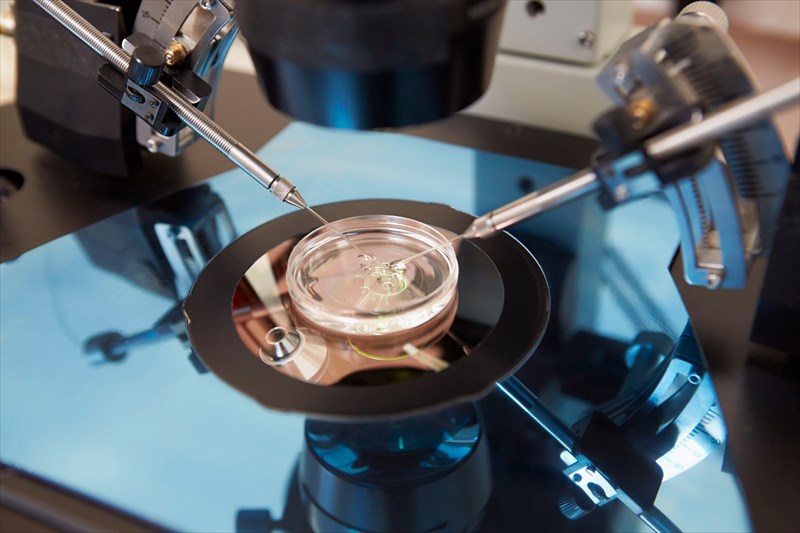
- In vitro maturation (IVM): This technique involves harvesting immature eggs from a woman’s ovaries. Harvesting can be done from unstimulated or minimally stimulated ovaries with the assistance of ultrasound scan guidance. Maturation of these eggs then happens in the laboratory (in vitro) for between 24 and 48 hours before the fertilisation process takes place. Maturation involves the use of a culture medium consisting of small quantities of hormones. Fertilisation is then done by ICSI (Intracytoplasmic sperm injection), a process whereby a single sperm cell is injected directly into a viable egg and viable embryos are then implanted in a woman’s uterus. The IVM technique also reduces the risk for OHSS (ovarian hyperstimulation syndrome), is less costly and doesn’t involve as much medical monitoring. The stages of treatment are also shorter which may be ideal for women unable to tolerate the effects of medications necessary for stimulation or for those with PCOS (polycystic ovarian syndrome). It has also proved successful for younger women (aged 35 and younger) with normal menstrual cycles.
There are also different techniques involved in the embryo transfer process. These include:
- Fresh embryo transfer: Once eggs have been harvested and fertilised (cultured) in the laboratory for 1 or 2 days, the best quality embryos (usually between one and three) will be selected for transfer to a woman’s uterus. These embryos will usually have a higher chance of success. For women under 40, at least 3 embryos can be implanted (some countries have strict rules prohibiting more than three, while others are more relaxed). The more viable embryos are implanted, the higher the risk of multiple foetuses occurring.
- Fresh blastocyst transfer: This technique involves an embryo culture in a laboratory incubator before the fertilised eggs are transferred to a woman’s uterus. The fertilisation process may take a few more days (up to 5 or 6 days) than the fresh embryo transfer in order to see if they develop into blastocysts (a mammalian blastula – meaning ‘sprout’ / embryo in which some differentiation of cells takes place in early development). Success rate for this transfer technique are higher than the fresh embryo transfer method.
- Frozen embryo (or blastocyst) transfer (FET): Those fertilised embryos which are not used during the fresh blastocyst transfer method during a treatment cycle may be frozen for future use. The benefit of doing this is that a woman may not need to undergo another stimulation process to harvest more eggs from her ovaries. She may do this for a repeat treatment to try and fall pregnant or attempt to use these for a future pregnancy down the line. Once a woman’s body is able to undergo another treatment (and has recovered), frozen embryos can be implanted for another treatment cycle.
- Assisted hatching: Some specialists may thin out (or weaken) the outer layer (zona pellucida) of a fertilised embryo as a way to assist it with ‘hatching’ once implanted in a woman’s uterus. Currently, there is no conclusive evidence that this technique increases IVF success rates, however some success has been achieved in the past. If several cycles have been unsuccessfully tried, some specialists may recommend this technique to try for a potential pregnancy.
