
How does IVF work?
It’s important to understand that not every treatment cycle will result in a successful pregnancy. For this reason, the option to freeze any unused (viable) embryos is becoming common practice in many clinics around the world.
Depending on a woman’s / couple’s situation, IVF treatment can make use of:
- A woman’s own eggs and a partner’s sperm
- A woman’s own eggs and the sperm of a donor (a known person who isn’t a partner or that of an anonymous individual)
- Eggs from a known or anonymous donor and a male partner’s sperm
- Eggs from a known or anonymous donor and an anonymous male sperm donation
- Donated embryos (donor eggs and sperm)
How it all begins…
When a woman intends to fall pregnant, the first port of call should be a visit to her general practitioner (GP). Here, a doctor can take note of a woman’s entire medical health history, conduct a thorough physical examination, and if necessary advise any changes to lifestyle (which may influence a potentially successful and healthy pregnancy) or recommend a variety of tests as he or she sees fit. These can check for potential abnormalities or rule out any possible concerns.
Your GP is also likely to refer you to a fertility specialist if you do not already have one in mind. A fertility specialist will review all history and assessment information before determining what options are available to you. It may be that a specialist will not outright recommend IVF treatment initially. There may be other options to try before invasive methods such as IVF.
Preparations for IVF treatment
Specialists may also conduct their own assessments which will include a comprehensive interview outlining a medical and social history, as well as a series of screening tests and profiles for analysis.
Screenings which will be done in preparation for IVF treatment include:
- Ovarian reserve testing: A specialist will need to assess the quality and quantity of a woman’s eggs. To do this, specialists test FSH (follicle-stimulating hormones) concentrations, as well as oestrogen (oestradiol) and anti-mullerian (AHM) hormones in the blood. This is done during the first few days of a woman’s menstrual cycle and is needed for assessing possible difficulties in retrieving eggs. The profile will also look for potential hormone imbalances (if applicable). The results of this analysis are usually paired with an ultrasound scan of the ovaries. Together, a specialist can then assess how the ovaries are likely to respond to stimulating medications, as well as gain a very good idea about the size and quality of eggs available for use.
- Uterine cavity exam: An examination of a woman’s uterine cavity is important for a specialist to assess before IVF procedures commence. The examination may involve a sonohysterography, where fluid is injected into a woman’s uterus through the cervix, and an ultrasound scan is done. Some specialists may also include a hysteroscopy which involves a flexible telescope (hysteroscope) that is inserted through the vagina and cervix in order to reach the uterus for examination.
- Infectious disease screening: Various infectious diseases such as HIV/AIDS, and hepatitis B and C will need to be screened for. A specialist will also want to test a woman’s immunity to Rubella (German Measles) via a blood sample before proceeding with the treatment procedure as this disease can cause a variety of complications during early pregnancy including miscarriage and stillbirth as well as birth defects in the developing foetus.
- Semen analysis: This screening is often done during an initial fertility evaluation, but may also be done shortly before an IVF treatment cycle.
- Practice (or mock) embryo transfer: A mock embryo transfer may be recommended as a way to assess the depth of a woman’s uterine cavity. The technique can help to successfully implant embryos when it comes time to perform the actual procedure.
Once assessments have been done and analysed, things begin to enter a decision-making phase. It is at this point that most may find they begin to have a lot of questions. Specialists can help to address any and every question relating to the treatment process and all possible outcomes.
Some important questions relate to:
- The number of embryos which will be implanted during an IVF cycle: This may depend on a woman’s age, as well as how many viable eggs were harvested (retrieved for fertilisation). The older a woman is, the higher the number of embryos for implantation will be recommended so as to increase the chances of a successful pregnancy. There is a limit, however, as many countries around the world have strict regulations when it comes to the number of embryos that can be implanted during a single cycle. A fertility specialist will be well aware of all regulations and restrictions, and advise accordingly. If using donor eggs, numbers may also be limited for implantation use. It is best that a number is agreed upon by all before commencement of treatment.
- Extra / left-over embryos: It can happen that all eggs that are collected are not used, even if viable for implantation. Any extra (viable) embryos can be discarded, or frozen and stored for future use. It is important to take into consideration the success rates of frozen embryos as opposed to freshly used ones. When freezing embryos, a successful pregnancy is not impossible (although odds may be slightly lower), but not all frozen embryos survive the cryopreservation process (freezing and thawing). There is also the option to donate unused frozen embryos, either for research purposes or to another IVF candidate wishing to try and conceive.
- The possibility of multiple pregnancies: A cycle of IVF has been known to result in multiple pregnancy – twins, triplets etc. The reason is that more than one embryo is usually transplanted in the uterus at a time. Not every transfer process will result in multiples, but it can happen, and thus should be carefully taken into consideration before treatment. A specialist can discuss, in detail, what the odds are and also advise how best to handle this possibility.
- Potential risks and complications: If using biological components (donated eggs, sperm or fertilised embryos), or a gestational carrier, it is best to take all risks, complications and possibilities into careful consideration. The treatment process alone is as much an emotional journey as it is a physical one. Adding in the use of biological components that are not your own can make the process just as emotionally taxing. Legal implications may also need to be taken into consideration in this regard. It is best to resolve all possible risks or concerns before treatment commences.
Counselling may be recommended at this stage if a candidate feels it may help to either make a decision to go ahead with treatment, or assist with dealing with the invasive nature of what is soon to take place.
Going through IVF is not only physically invasive, it can also be emotionally straining too. Depending on the reasons for going through this means of trying to conceive, counselling can be very effective in preparing a single woman, or couples, for their experience.
Counselling may also be effective in helping a person cope with the financial implications of undergoing treatment. There is no guaranteed price tag for a cycle of IVF. Candidates circumstances vary from one to the next. Options available can help to tailor the treatment process, and finances can be taken into consideration during this process (some options work out cheaper than others).
Weighed against biological factors, expenses can become overwhelming. If counselling helps to deal with the impact of this, it is wise to make full use of it before starting treatment.
IVF procedure stages
The standard process of an IVF cycle involves several stages which can take at least two weeks from start to finish (sometimes a little longer). Multiple attempts can be time-consuming and depend on a variety of different factors.
The stages involved are:
Ovulation induction (stimulation or super ovulation): If opting for ovulation stimulation techniques, this will normally be the first stage of IVF treatment. This involves the use of synthetic hormones (that mimic the natural process) to help stimulate a woman’s ovaries to produce multiple eggs (usually these only produce one egg during a menstrual cycle) and suppress the natural cycle. Ovulation helps to prepare the body for a potential pregnancy. Multiple eggs are needed as not all eggs will be viable for use. Some will fertilise and others not. Stimulation medications may include injectable (or nasal sprays) FSH and luteinising hormones (LH), human chorionic gonadotropin / HCG (usually taken after 8 – 14 days once follicles are near ready for egg retrieval), followed by drugs to prevent the body from releasing eggs prematurely, as well as others, such as progesterone supplements, which will help to prepare the lining of the uterus for the retrieval stage. A specialist will advise a woman as to the correct ways to administer injections effectively throughout, and also how to monitor doses. This initial stage can take between 1 and 2 weeks before moving on to the next stage. Throughout the stimulation process, blood tests and ultrasound scans may be frequently required, so a woman can expect fairly regular consultations with her specialist to be certain that harvesting (the next step) can take place. A vaginal ultrasound will be done to assess the development of follicles and whether the eggs are mature enough for retrieval. Blood tests will be used to assess levels of oestrogen (which should be higher at this stage) and progesterone (which should remain low) once ovulation has occurred. If at this stage there are an inadequate number of follicles (or too many), or eggs are released prematurely, the IVF process may go no further. In this case medications may be adjusted and the stage repeated.
Women - Egg harvesting (retrieval) / ‘follicular aspiration’: Within 34 to 36 hours following successful stimulation, the next stage will take place. A woman will be lightly sedated and given medication for pain or discomfort. Many specialists opt for a transvaginal ultrasound aspiration method of retrieval whereby a thin probe is inserted into the vagina (for follicle identification), followed by a needle (with a suction device) to be used as a guide to reach the follicles and harvest the eggs. Abdominal surgery or a laparoscopy are other methods which can be used should the ovaries not be accessible enough. In this instance, a small incision is made near the navel and a laparoscope is inserted to help guide the needle used to retrieve eggs. Either retrieval process usually takes about 20 minutes to complete. Harvested eggs are then placed in a culture medium (nutritive liquid) and incubated. Those that are viable will be used in the next stage. A woman may be given medications to assist in preparing the uterus for implantation while fertilisation occurs. If necessary, a pessary may also be given (a medical device used to prevent uterine prolapse).
- Men - Sperm retrieval / donation: If applicable, a candidate’s partner will need to provide a semen sample (through masturbation) on the morning of egg harvesting. Sperm can also be surgically extracted, directly from the testicle if necessary (normally if there is a blockage that prevents sperm from being ejaculated). Once a sample is collected, sperm is separated from the semen fluid in the laboratory (from a partner, as well as from an anonymous donor). Donor sperm will be taken out of storage and thawed for the fertilisation stage.
Fertilisation / insemination / embryo culture: The two most commonly used fertilisation methods are insemination (healthy sperm and mature eggs are mixed and then incubated overnight with careful atmospheric, temperature and infection control) or ICSI (intracytoplasmic sperm injection – a single healthy sperm is injected directly into one egg at a time). ICSI is typically used when semen quality is poor or previous fertilisation attempts have failed. It is at this stage that pre-implantation genetic testing (which can also assess the correct number of chromosomes as well as various disorders) or assisted hatching techniques may take place (if applicable). Once eggs and sperm have been fertilised, they will be monitored in the laboratory to assess whether they are viable for implantation.
Embryo transfer: Within 2 to 6 days of egg harvesting (or 3 to 5 days following successful fertilisation), the embryo transfer stage will take place. A woman will, again, be given a mild sedative (remaining awake but relaxed) to help ease discomfort (usually mild cramping). Once ready, a speculum will be placed to hold the vagina open and a catheter (long, flexible tube) will be inserted into the vagina, through the cervix and into the uterus. Using a syringe, one or more (up to 3, depending on a woman’s age and country laws) fertilised embryos suspended in a small amount of liquid will be attached to the end of the catheter and passed through the tube. Embryos will then be placed into the uterus so that they can implant in the lining of the womb. Implantation in the uterine lining can take anywhere between 6 and 10 days to successfully occur, resulting in a pregnancy.
What happens after the procedure
IVF treatment does not require hospitalisation and is usually performed as an outpatient procedure. A woman can resume normal daily activities shortly after retrieval and implantation procedures.
Upon completion of implantation (embryo transfer into the uterus), a woman’s ovaries may remain enlarged for a short period of time. A specialist will advise a woman to avoid any vigorous activity following both harvesting and transfer procedures. Complete bed rest is not usually necessary, unless a woman is at risk of OHSS.
The invasive nature of the procedure is not without some short-term side-effects for a woman undergoing IVF. These can include:
- Mild bloating and cramping
- Breast tenderness (as a result of higher than normal oestrogen levels)
- Constipation
- Passing a small amount of fluid, which may be clear or bloody (shortly after the transfer procedure)
Specialists will also likely prescribe hormone medications to be taken daily for between 8 and 10 weeks, either in pill form or as injections. Normally, progesterone is naturally produced in the body to assist with preparing the body for pregnancy (assisting with successful implantation) by thickening the uterus lining. If there is too little of the hormone in the body during the early weeks of pregnancy, miscarriage occurs. Medication can help to prevent this.
If a woman experiences any severe discomfort or pain (especially in the pelvic area), a high fever, or heavy bleeding (including blood in urine), she should contact her specialist / doctor as soon as possible. He or she will then need to examine for any potential complications. These can include things like an infection, severe ovarian hyperstimulation syndrome or ovarian torsion (twisting of the ovary).
After about 12 to 14 days following the transfer procedure, a specialist will wish to see the woman for a follow-up consultation. It is at this stage that she will be tested for pregnancy.

 Ovulation induction (stimulation or super ovulation):
Ovulation induction (stimulation or super ovulation): Women - Egg harvesting (retrieval) / ‘follicular aspiration’:
Women - Egg harvesting (retrieval) / ‘follicular aspiration’: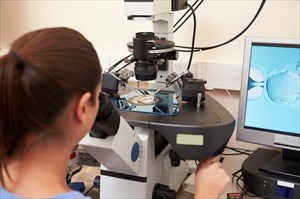 Fertilisation / insemination / embryo culture:
Fertilisation / insemination / embryo culture: Embryo transfer:
Embryo transfer: