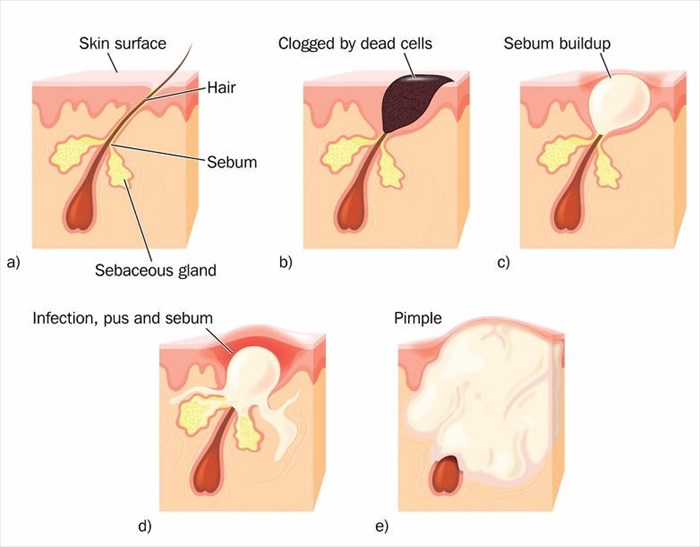
Defining Acne
Acne (acne vulgaris) is one of the most common skin conditions around the globe. It occurs when oil, bacteria, dirt and dead skin cells clog up the tiny pores in the skin. The result is what’s commonly referred to as blemishes, whiteheads, blackheads, pimples or zits.
If the skin is repeatedly affected by continuous clogging, you may have acne. This condition can be reasonably mild (just a few spots) or more severe (many spots covering the face, neck, chest and back which can be small or bigger, more solid and inflamed lumps or cysts that can be painful).
Acne is a common condition among teenagers when hormonal changes in the body are rife. Many experience bouts of acne which then subsides as hormonal levels stabilise following the teenage years. Some women experience acne as adults (even those who did not have the skin condition in their teens), often in the days leading up to their menstrual periods as well as during or after pregnancy.
When severe, an acne condition can be quite distressing for a person. How you feel about your condition is not necessarily only related to how bad or severe it is, many males and females are bothered or embarrassed about it even when in mild form. Others, even if severe, will not be upset about it at all.
Acne typically affects the face and for this reason, the condition can impact a person’s self-esteem. Over time, severe acne can also lead to scarring which can cause further emotional distress.
The important thing to remember about acne, is that although it can be persistent, the condition is not life-threatening. It can be painful and distressing, but for many it can be treated or adequately managed. Treatments can effectively reduce the number of blemishes and your chances of physical scarring.
Other Articles of Interest

Birth Control
Preventing an unwanted pregnancy is simple to do and comes down to your preferred method. We breakdown the different types, and pros and cons of each ...
Stress
Stress can affect everyone differently. It is your body's biological response to a certain situation. It is important to know how to deal with stress in order to develop certain coping mechanisms...

Chemical Peels
Chemical peels in one form or another have been around for over 60 years. In the quest for ever youthful, beautiful and glowing skin, we explore the various aspects of these beauty treatments...