What is diverticulitis?
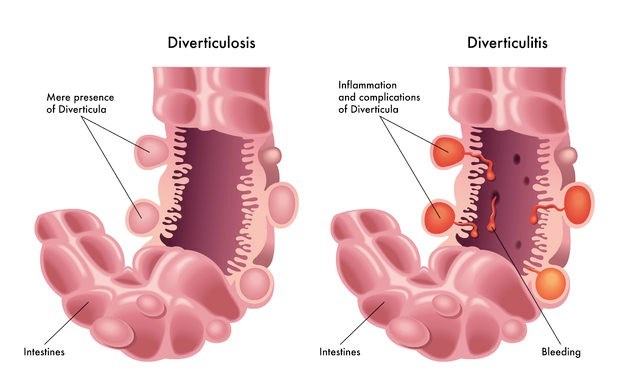
Blisters or sacs form when the inner layer of the digestive tract is forced through weak areas in the outer layer. Diverticula can, theoretically, occur anywhere between the mouth and the lower portion of the large intestine (colon), where blood vessels run through the intestinal wall.
These blisters may occur without infection and are most common in individuals over the age of 40 (rarely causing any problems). Many with uninfected blisters may be oblivious to having them as no symptoms are present. The condition in this instance, is known as diverticulosis. To date, it is not fully understood why some diverticula become infected and others do not.
Infected diverticula may occur anywhere in the digestive tract. A tell-tale sign is a painful sensation in the lower left side of the abdomen, and rectal bleeding. Most often pain and bleeding is accompanied by other signs of infection such as fever, nausea and a distinctive change in normal bowel movements.
Diverticulitis is a treatable condition, but a person can experience recurring infections and / or diverticulosis (diverticular disease). The disease can be mild or severe (recurring), and is treated accordingly.
Other Articles of Interest

X-rays
X-rays are a very common procedure that many of us have had to have or may have in the future. If you want to know more about the imaging test, read all about it here.

Fever (Temperatures)
Often a sign that something is wrong in the body, a fever is a typical symptom of a variety of different illnesses. When should you worry? Here's all you need to know...

Irritable Bowel Syndrome (IBS)
IBS is a common and often uncomfortable condition, if you want to know more about it, read our article.