
What is irritable bowel syndrome (IBS)?
Irritable bowel syndrome, commonly known as IBS but also occasionally referred to as irritable colon, spastic colitis, spastic colon and mucous colitis, is something many people experience. The word 'syndrome' refers to a group of conditions or symptoms that occur simultaneously. With IBS, the syndrome is a chronic gut disorder that affects the gastrointestinal tract, and predominantly the large intestine.
It is estimated that approximately 11% of the global population suffers from IBS, with prevalence noted in developed, westernised countries1.
The majority of the global IBS demographic are women, although it also affects men. IBS sufferers also tend to have a family history of IBS.
IBS can be an uncomfortable and often painful condition. Although it is not life-threatening, it can take a major toll on sufferers lives, often forcing them to plan their lives and social activities around flares, which always worrying about unpredictable bowel movements or pain.
As common as the condition is, doctors are still unsure of the exact cause of irritable bowel syndrome. It is, however, important to note that this condition is not in any way related to inflammatory bowel disease or any other bowel conditions. It also does not increase the risk of gastrointestinal cancers.
References
11. Card T, Canavan C, West J. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014:71. doi:10.2147/clep.s40245
Other Articles of Interest
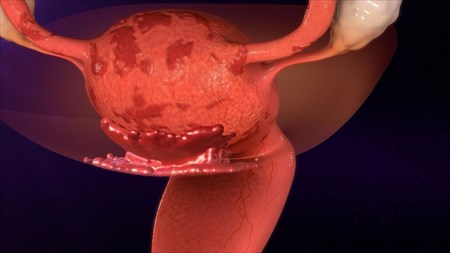
Endometriosis
Endometriosis can be a painful condition that many women suffer from. However, it does not have to be a debilitating one. What is it? Find out here...

Gastroenteritis
Gastro, which is often known as the 'stomach flu' can be a painful and oftentimes common condition. Most people are able to recover without treatment. Here's everything you need to know...

Coeliac (Celiac) Disease
Coeliac (Celiac) disease is something more and more people are being diagnosed with. Many people may not realise they have the condition, find out what you need to know...
