How would smallpox infections be treated or prevented?
There is no official treatment regimen for smallpox infections. To date, the primary means of dealing with the condition has been through aggressive vaccination to eradicate epidemics and provide supportive care to alleviate symptoms of the infection. If an outbreak had to occur, it is more than likely that health organisations would focus on using the vaccine in order to eradicate the spread of infection once again, rather than attempt to do so with the use of antiviral medications (although these would be used in a supportive capacity to alleviate some symptoms).
Supportive care (hospital / clinical care)
This would involve the following:
- A patient would be placed in isolation (in a designated room with negative pressure – air flow is allowed into the room, but none can be permitted to leave it – thus reducing respiratory risk or transmission contact) until all scabs have been shed from the body and the person in question is no longer considered contagious. The room must be equipped with private bathroom facilities and must not share any ventilation systems with any other part of the hospital.
- A patient’s electrolyte and fluid levels will be constantly monitored and sufficiently maintained so as to prevent dehydration.
- Care will be taken to provide a nutritious diet throughout the isolation period.
- Symptoms of pain and fever will be alleviated with recommended medications. Any skin discomforts experienced will also be managed. Any lesions which affect the cornea of the eye will likely be treated with topical idoxuridine (an antiviral medication).
- Daily monitoring of the patient’s overall condition will be undertaken so as to prevent or treat any complications which may arise. A patient with a fever will have readings taken at least twice daily. If a fever spikes, public health officials are required to be notified. An infectious disease specialist will likely form part of the care team monitoring and treating the patient.
- Should a smallpox infection not be confirmed by the laboratory, a patient is still likely to receive a smallpox vaccination to curb any risk of accidental transmission.
It is important for a patient to be isolated so as to prevent the risk of transmission of the disease, particularly to any unvaccinated individuals. It is also important to ensure that a patient is sufficiently cared for and made comfortable while in isolation.
Any medical personnel providing care to an infected patient will wear protective clothing, respirator / surgical masks and eye masks. Just before leaving the isolated area, all protective clothing will need to be removed and placed in the available biohazard disposal containers. This helps to reduce risk of spreading the infection into other parts of the hospital. Disposed items will be incinerated or decontaminated with ethylene oxide. Anything reusable may be soaked in hot water and bleach.
Anyone handling a patient and his or her clinical samples, clothing or bedding, will be tested for immunity or appropriately vaccinated.
If a large outbreak had to occur, the CDC has recommended that designated clinics or hospital environments be set up in the relevant regions in order to provide sufficient supportive care. Alternatively, at home care can be considered with strict guidelines and precautions. Non-hospital isolation will need to be authorised by the public health officials of the country / region concerned.
Some factors which could permit non-hospital / home care isolation include:
- The infected patient not requiring constant medical monitoring and having the ability to remain sufficiently hydrated and nourished on their own.
- A non-hospital environment being fitted with the appropriate climate control functionality (heating or air conditioning) and not sharing any ventilation systems. This environment will also have its own bathroom facilities and running water.
Should a patient require transferral from one isolation room to another, precautions to reduce contact or respiratory risk will be implemented (i.e. the wearing of surgical mask, gloves, body coverings etc.).
Once the patient is no longer contagious, a doctor will assist in providing care for cosmetic scar management and recommendations for correcting or managing any impairments of vision experienced as a result of the infection.
Medications
Currently there are no classified medications approved for specific smallpox infection treatment. Other FDA (US Food and Drug Administration) approved medications can be used (off label) to help manage any infections. Medications have not been adequately studied for human efficacy, specifically in relation to smallpox infection treatment, as there has been no need for this. Thus, if ever a smallpox outbreak occurs, a doctor will carefully assess the risk of using any medication off label over its possible benefits. Options available which may be considered include:
1. Antivirals
- Cidofovir (Vistide): This medication is approved for CMV (cytomegalovirus) treatment and is classed as a viral DNA polymerase inhibitor. Animal research has shown some benefit in treating Orthopoxvirus infections but has not yet been researched in humans infected with VARV. (8) A doctor may recommend Cidofovir analogs CMX001 or the extracellular virus inhibitor ST-246 in the case of suspected smallpox infection.
- Idoxuridine (Herplex): This medication is classed as an analog of thymidine which is currently approved for topical use in the treatment of CMV retinitis. If a patient has any ocular problems as a result of a smallpox infection, this medication may be considered as a means to try and prevent further viral infection capable of destroying tissues.
The medication, Tecovirimat has been researched and tested as a possible option for the treatment of smallpox infections. Animal testing has shown some promise. The drug is yet to be effectively tested in individuals with a smallpox infection. For the time being, minor side-effects have been experienced by uninfected individuals temporarily on the drug. (9) Another experimental medication is Brincidofovir, which is being tested for treating infections caused by adenovirus, smallpox, cytomegalovirus and Ebola.
2. Antibiotics
Should any secondary bacterial infections of the skin occur while under care, the following medications may be prescribed for treatment:
- First generation cephalosporins (Cefazolin or Cephalexin) or Clindamycin
- Semisynthetic penicillin medications (Nafcillin, Dicloxacillin, Oxacillin or Cloxacillin) and Ampicillin (Sulbactam) or Amoxicillin (Clavulanate)
Vaccination
The smallpox vaccine is currently the most successful way to control the disease and keep infection rates at their ideal lowest (zero). Should a person be exposed to VARV, vaccination within at least 3 to 4 (or up to 7) days following exposure will help to ensure a significantly lower risk of infection or considerably reduce the severity of symptoms after the incubation period. Should a new case of smallpox be officially diagnosed, anyone with exposure risk should seek a vaccination to benefit from this preventative method.
.
A brief history of vaccination efforts
A fever and rash typically developed in recipients following variolation, however, fewer deaths were noted in individuals who underwent this procedure than in those who had contracted the disease naturally.
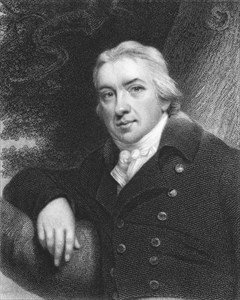
Steps to develop a vaccination for the disease officially began in 1796. An English physician, Edward Jenner had observed that infections with cowpox did not present the same symptoms of smallpox following variolation. He began experimenting with the contents of cowpox sores and the variola virus and found that his participants did not develop smallpox symptoms.
In 1801, he published his experimental findings (called ‘On the Origin of the Vaccine Inoculation’) which showed that the virus causing smallpox could be used as a successful control method of the disease, providing immunity. Soon after, the practice of vaccination replaced variolation. During the 1800s (the precise date is seemingly unknown), the cowpox virus was replaced with the variola virus as the primary vaccine material.
In 1951, the WHO initiated a global eradication programme, which unfortunately encountered a few hiccups in terms of funding, vaccine donation shortages, lack of personnel and country participation commitment (particularly in endemic countries). Outbreaks were still problematic during the 1960s. The bifurcated needle was developed in 1961 which made vaccine administration simpler to perform and therefore more efficient as well as cost effective.
By 1967 the programme was given a boost and efforts were intensified. Steady progress was made through the 1970s until the official eradication announcement in 1980. The only risk now, is that a growing percentage of the global population is not immune to smallpox, which could present future health concerns should there ever be an outbreak once again. Precautionary measures involving vaccine stockpiles have been implemented for this reason, offering a safety net for disease protection.
Vaccinia vaccine (live / viral)
The vaccinia vaccine (Dryvax) ensures immunity against VARV by activating antibodies and is one of two licensed vaccines (approved by the FDA in 1931). The vaccine comprises of a live vaccinia virus (not variola) which is another member of the Orthopoxvirus family, but one that is less harmful. As the vaccine contains a live virus, precaution must be taken with both the administration and after care of the inoculation site (usually the arm) so as not to spread the pathogen to another part of the body.
Once a person is vaccinated, a mild infection and an immune reaction is induced in the body (activated antibodies) as a means to fend off infection and provide sufficient immunity. The vaccination does not cause a serious smallpox infection.
The vaccine is administered by what is known as a scarification method. This involves the use of a bifurcated needle (a narrow, steel needle that is approximately 6cm long and has two prongs at one end) that is dipped into the vaccine. The prongs are designed to ‘hold a dose’ of the vaccine once dipped. The tip of the needle is then pricked or poked into the skin of a recipient (not too deeply). A total of 3 doses are given during an initial vaccination. If a person is being vaccinated again, at least 15 doses are given. The vaccination process is short, taking a minute or two at the most and is relatively painless.
The medical professional administering the vaccination will assess a recipient within 3 days to determine whether or not the process has been effective. If a visible papule develops within 3 days and progresses to the pustular stage within 7 to 10 days, the vaccination will be considered successful. A resulting scab shedding by a least 21 days following vaccination will then likely take place, completing the process. If a recipient is being re-immunised, the pustule formation and scab separation may take place a little sooner (shedding by around day 14).
An alternative to Dryvax is vaccinia virus vaccine ACAM2000 which received FDA approval in May 2017 and is now also licensed. (10) ACAM2000 also contains the live vaccinia virus and induces the same mild infection and immune reaction with one dose, administered through the skin. ACAM2000 is a necessary alternative as Dryvax is now in limited supply due to a halt in manufacturing. The vaccine has also been shown to work effectively as an immunisation booster in individuals who have received a vaccination before. A dose given to a recipient who is at risk of exposure but has not yet developed a rash can also provide effective immunity.
For the time being, ACAM2000 is not indicated for use in individuals who have severely compromised immune systems. Next-generation vaccines are being researched as possible alternatives in this regard. Some on the radar include LC16 and Imvamune (Bavarian Nordic) – neither of which are yet approved or licensed.
Post vaccination, immunity is estimated to be 95% successful for at least 3 to 5 years but may begin to decline somewhat thereafter. Long-term protection which may be required for certain individuals, such as the military and healthcare personnel, can be acquired through booster vaccinations. Routine vaccinations for the general public have not been required since the official eradication of the disease.
Vaccinia immunoglobulin (VIG)
Passive immunity may, on occasion, be recommended when the vaccinia vaccine cannot be used, such as in the case of individuals with compromised immune systems who may be at a higher risk for further complications.
VIG involves the administration of antibodies (derived from plasma) taken from a successfully immunised individual and given to a person who is not immune to the virus causing smallpox. This procedure, which is only facilitated through the CDC, can provide some temporary immune protection against VARV and is FDA approved to be given intravenously (VIGIV or CNJ-016).
Although considered rare, VIG may be used in the event of vaccinia-related complications, like vaccinia necrosum (also known as gangrenosum or progressive vaccinia) which can occur when the inoculation site fails to heal, causing progressive necrosis (cell death). Another complication may be eczema vaccinatum, which causes a severe / extensive rash.
Vaccination side-effects
Some inflammation and redness (erythema) can be expected near the inoculation site (accompanied by a little soreness), as well as a mild fever, swollen lymph nodes (glands in the armpits), body aches, headache and general malaise. First time vaccination recipients may experience stronger reactions than those receiving a re-vaccination or booster shot.
Most individuals, however, are not expected to have severe side-effects, but these may occur. Some individuals may have serious or even life-threatening reactions to the live viral vaccine.
Before administering a vaccine, a doctor will have already assessed whether a person is at increased risk for a possible severe reaction or not. Some factors that will be taken into consideration include:
- Existing chronic skin conditions (like eczema or atopic dermatitis)
- Active breaks in the skin (such as in the case of acne)
- A compromised or weakened immune system (due to conditions such as HIV/AIDS and cancer, following an organ transplant or after having taken a course of certain medications, like steroids which can suppress the immune system)
Adverse reactions which may occur in a very small percentage of the population receiving vaccinations will require medical intervention (treatment). More severe reactions, some of which may be life-threatening, can include:
- Vaccinia virus spreading – if the inoculation site is touched and other portions of the body are subsequently touched, spreading of the virus can occur, resulting in more symptomatic reactions. All vaccinated individuals would have been cautioned in this regard and advised to thoroughly wash their hands with soap and warm water should any contact be made in the days following immunisation.
- Allergic reactions, such as a rash on the body.
- Widespread skin infection, such as eczema vaccinatum (this is more common in individuals with pre-existing / chronic skin infection conditions)
- Tissue inflammation around the inoculation site – a build up of tissue can result in progressive vaccinia, producing large and non-healing lesions / sores. Such a reaction is more likely to be seen in individuals with compromised immune systems.
- Postvaccinal encephalitis (PVE) (inflammation of the brain after receiving the vaccine)
- Myocarditis (inflammation of the heart)
- Pericarditis (inflammation of the lining of the heart)
- Myopericarditis (a combination of myocarditis and pericarditis)
There have been instances where chest pain (angina), shortness of breath and heart attack have occurred, but it is not clear as to whether these were isolated events or related to the vaccination in any way.
When would a vaccination against smallpox be required?
An emergency reserve stockpile consisting of at least 31 million doses held by donor countries, including France, Germany, Japan, New Zealand and the US has been pledged to the WHO for international use should outbreaks arise and the vaccines be required. (11)
For the time being there is no official requirement for people to receive routine smallpox vaccinations while the disease is considered eradicated.
Certain individuals, however, are advised to receive vaccination even when there is no reported outbreak, mostly due to their line of work. These individuals include laboratory technicians who handle the live virus (or others belonging to the same family) and certain members of the military. Vaccination thus reduces risk of infection and subsequent illness. Booster vaccinations may be required every 3 years) should more long-term immunity be required.
If there had to be an outbreak of smallpox, vaccination strategies would most certainly change and become mandatory, particularly if a person has been directly exposed to an individual confirmed to have the virus. An outbreak is likely to be considered an international health emergency.
Depending on the nature of the outbreak, public health officials will issue guidelines and requirements obtained from the CDC advising on the course of action for local authorities to implement in their respective regions or countries. These guidelines will be aimed at providing maximum protection in order to prevent the spread of infection and regain control over the disease. Control is likely to be regained by means of routine vaccination and not pharmacological products.
Strategies would also likely focus on the sufficient isolation of infected individuals and administration of supportive care during their illness. Should there be any reported deaths as a result of smallpox re-emergence, cremation of the bodies would likely be required. Surveillance monitoring strategies would also be implemented in any instances where it is known that certain individuals may have been exposed to the virus. All cases of suspected or confirmed smallpox infections will be expected to be reported to the CDC.
Care guidelines for the inoculation site
The use of a live virus does carry the risk of the spread of infection and thus, the inoculation site must be properly cared for following vaccination. Merely touching the site before healing is complete (whether it be with the physical body, clothing or bandages etc.) can spread the virus to other portions of the body, which will result in illness.
Guidelines for care include:
- The inoculation site must be loosely covered with a gauze bandage and secured with tape or plasters that are semi-permeable (allowing air to flow through but not fluid contents).
- Sleeved shirts should be worn in the days following vaccination, providing more protection to the site while healing takes place.
- The inoculation site should be kept dry while healing. If the protective covering (bandage or clothing) does get wet, these should be changed right away.
- While bathing, waterproof bandages should be used to help keep the site dry. Towels used to dry off after bathing must never be shared with another individual.
- Protective coverings (bandages) should be changed at least every 3 days (sooner if they encounter dirt or moisture).
- Practicing good hygiene is encouraged, especially while the inoculation site is healing. A vaccination recipient or any other individual must not touch the site. Precaution should be exercised where contact can be made with other items or objects – direct contact can cause contamination and run the risk of spreading the virus and causing infection.
- Bed linens, clothing, towels etc. must all be laundered separately from those used by others and washed with hot water, detergent or bleach.
- Used bandages and protective coverings, as well as the scab that is shed must be placed in zip lock bags and disposed of (when being discarded with regular trash).
References:
8. US National Library of Medicine - National Institutes of Health. September 2013. Orthopoxvirus inhibitors that are active in animal models: an update from 2008 to 2012: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929309/ [Accessed 06.04.2018]
9. ClinicalTrials.gov. 7 June 2015. A Trial to Assess the Safety, Tolerability, and Pharmacokinetics of the Anti-Orthopoxvirus Compound Tecovirimat (SIGA246-008): https://clinicaltrials.gov/ct2/show/NCT02474589 [Accessed 06.04.2018]
10. US Food and Drug Administration. March 2018. ACAM2000: https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm180810.htm [Accessed 06.04.2018]
11. World Health Organization. December 2017. Smallpox Vaccines: http://www.who.int/csr/disease/smallpox/vaccines/en/ [Accessed 06.04.2018]
