Did you know? There are more than 100 different variations of arthritis and associated conditions.
Types of arthritis
‘Arthritis’ is characterised by similar symptoms, but is broken into various forms according to different causes and treatment methods. Many variations or arthritis or musculoskeletal conditions share similar characteristics.
As a result, arthritis conditions have been split into 7 main characteristic groupings:
Degenerative (or mechanical) arthritis
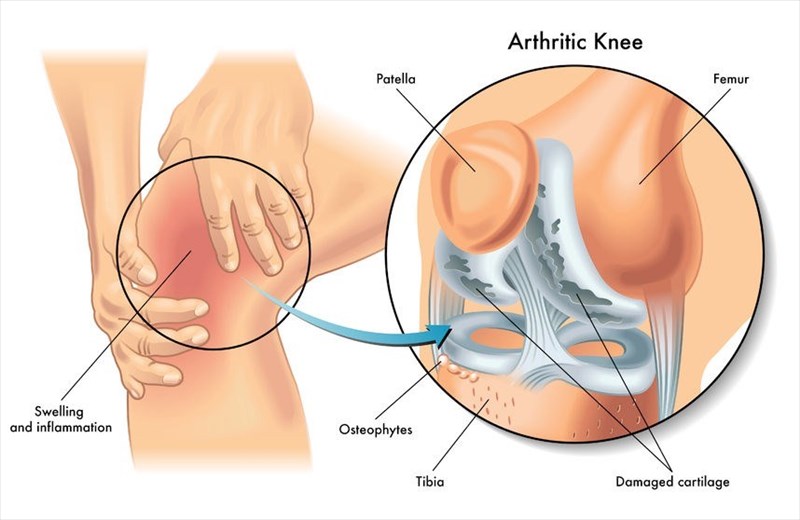
This category refers to those conditions which are characterised by damage to the cartilage that covers the ends of the body’s bones. The normal smooth surface of cartilage becomes rougher and thinner with damage. Bone effectively rubs against bone and wears away the slick, cushioning surface. The body reacts to this by attempting to restore cartilage stability and begins to ‘remodel the bone’. Osteophytes (bony growths) or misshapen joints may develop as a result. In the process, joints lose strength resulting in pain and stiffness. The most common form of this category is osteoarthritis (a wearing down of the flexible tissues at the ends of bones).
Inflammatory arthritis
Inflammation in the body is part of a normal, healthy healing process and defence against bacteria and viruses. When inflammation occurs without the presence of infection or injury, it causes distress to the joints and surrounding tissues, especially ligaments and tendons (enthesitis). The result is swelling, stiffness and pain. Inflammation can affect several joints in the body, causing erosive damage to the surface of the joints as well as underlying bone structures.
Types of inflammatory arthritis include rheumatoid arthritis, reactive arthritis (associated with infection), ankylosing spondylitis (this can lead to the fusing of vertebrae in the spine) and that which is associated with conditions such as colitis and psoriasis (psoriatic arthritis). These variations of arthritis are best diagnosed and treated early to prevent permanent damage to the joints.
Soft tissue musculoskeletal pain
This category variation refers to pain that is experienced in the joints, bones and surrounding soft tissues. This can happen as a result of an injury or overuse of specific areas of the body. Tennis elbow is one such example. Pain and inflammation effectively begins in the soft tissues and muscles which support the joints. When pain such as this becomes more widespread, the condition may be diagnosed as fibromyalgia.
Connective tissue disease (CTD)
Tissues, such as ligaments, tendons or cartilage, which separate, bind together or support the joints can become inflamed and lead to joint pain in the body. This can result as a symptom of CTD which can further affect the body’s muscles, kidneys, lungs and skin tissues as well. CTD can be broken down into further condition variations, all experiencing symptoms of joint pain, such as Systemic lupus erythematosus (SLE), Scleroderma (systemic sclerosis) or dermatomyositis.
Back pain
Pain and inflammation is usually associated with a specific cause and can originate in the body’s muscles, nerves, discs, ligaments, joints, bones, and even organs. All can result in sensations of referred pain. Osteoarthritis, arthritis in the facet joints of the vertebrae or a ‘slipped disc’ can result in back pain where inflammation and damage occurs in the spine.
Metabolic arthritis
Elevated levels of uric acid can accumulate and form needle-like crystals on the joints in the body. This can result in sudden bursts of severe pain or even a gout attack.
Uric acid is normally produced as a chemical when purines, found in the body’s cells and various foods, are broken down and dissolved in the blood. Most of the chemical will normally travel through the bloodstream to the kidneys, where it will be passed out of the body in urine. Some people naturally produce excess (more than the body needs or can get rid of during the breakdown process). When some of this remains, and accumulates, symptoms or arthritis can occur.
Sharp episodes of pain can affect a single joint or multiple joints in the body. Common areas where pain is experienced are the hands or a big toe (usually extremities that are not close to the warmest areas of the body).
Infectious and septic arthritis
Infectious arthritis typically develops if a virus, fungus or bacterium, such as salmonella or Shigella (food contamination), gonorrhoea or chlamydia (both sexually transmitted diseases), or hepatitis C (blood-to-blood infection) enters the body’s joints.
Septic arthritis typically affects the joints of the hips and knees and develops quickly, thus requiring prompt medical diagnosis and treatment. The infected joint results in inflammation and pain, but is usually treatable with antibiotics or antimicrobial medications.
Symptoms of arthritis can sometimes result in damage to the joints, causing chronic discomfort. These must be treated by a medical doctor as soon as possible to prevent extensive damage.
If damage is extensive, having persisted over a long period of time without appropriate treatment, it can be irreversible. Some existing conditions or treatment processes can increase a person’s risk of developing septic arthritis. These include chronic conditions such as sickle cell disease or diabetes, the use of artificial joint implants, medications that suppress the immune system, intravenous (IV) medications, joint arthroscopy (recent), or a joint injury (recent).
The most common forms of arthritis and associated conditions
Rheumatoid arthritis (RA)
Inflammation which persists in the synovia (the clear, lubricating fluid which is secreted in the joint cavities, tendon sheaths and the bursae cavities that counter friction in the joints) can cause cartilage and bone degeneration. This results in swelling, joint pain and sometimes joint deformity. Without adequate treatment, RA (an autoimmune disease, whereby the immune system ‘attacks parts of the body’) can severely compromise a person’s quality of life.
Osteoarthritis
This type of arthritis can develop gradually (over months or years) and is typically seen to worsen after the age of 40. Also a degenerative joint disease (leading to the breaking down of tissues), damage affects the entire joint, joint lining, ligaments and underlying bone. The most common areas affected are those that are most used (the ‘wear and tear effect’) – the knees, hands (especially the base of the thumb), hips, spine, and big toe joint. Without adequate treatment and careful management, osteoarthritis can become quite debilitating, especially for seniors during their later years. Essentially, the body’s natural ‘shock absorber’ is degenerated and worn down in the process.
Psoriatic arthritis
This condition often occurs as a result of an existing skin disease known as psoriasis (the build-up of skin cells that forms dry, itchy raised red and white patches and scales). This form of arthritis develops as an abnormal immune response in the body, adding to the overproduction of skin cells, and resulting in inflammation and symptoms of pain. Not all cases of psoriasis will develop psoriatic arthritis (generally only 10% to 30%).
Childhood arthritis
There are at least three variations of childhood arthritis classifications – JRA (juvenile rheumatoid arthritis), JCA (juvenile chronic arthritis) and JIA (juvenile idiopathic arthritis). All are typically diagnosed in children under the age of 16. The most commonly diagnosed is JRA.
Fibromyalgia
Widespread pain which also affects the body’s joints can cause additional symptoms of sleep disturbance, fatigue, and psychological distress. Abnormal pain processing in the body can result in severe chronic pain in the body.Many with fibromyalgia experience strong painful reactions to various activities that most would not experience any discomfort doing.
Causes of the condition are largely unknown, but can sometimes appear to be associated with PTSD (post-traumatic stress disorder), a genetic predisposition, problems with obesity, or conditions such as SLE, chronic fatigue syndrome and RA or viral infections and repetitive injuries.
Gout:
Joint pain is typically acute (red, hot and swollen) occurring in flares for several days or weeks. Gout (gouty arthritis) may go into remission for long periods of time and then flare up in chronic cycles of severe or agonising pain.
If chronic, it can develop into gouty arthritis. Risk factors that can lead to the onset of this condition include hypertension (high blood pressure), obesity or excessive weight, alcohol abuse, use of diuretics, or poor kidney function.
