How is a Cushing's Syndrome diagnosed?
It is more than likely that a diagnosis of Cushing’s syndrome will not be given in a single consultation. An initial consultation will focus on determining what symptoms are present, a medical history review and a physical examination. Thereafter, a doctor (usually a general practitioner or GP) will determine which tests may be necessary to either rule out certain medical conditions, which share a similar collection or symptoms, and then make a diagnosis.
Some questions a doctor may ask during a medical review include:
- What symptoms are you currently experiencing?
- How long ago did symptoms begin?
- Would you describe them as mild or severe?
- Have you tried any treatment methods that have appeared to either worsen or improve symptoms?
- Are you currently taking (or recently taken) any medications or supplements (including herbal)?
- If yes, how long have you been using these medications and supplements?
- Have you noticed that you are more emotional lately?
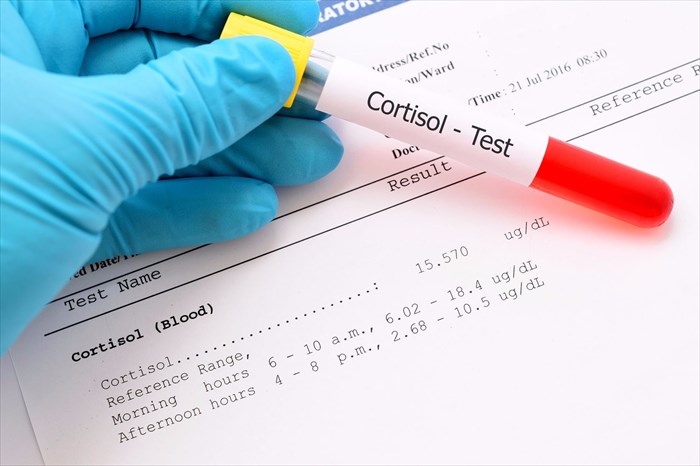
During a physical exam, a doctor will look for tell-tale signs of Cushing's syndrome, such as a ‘moon face’, buffalo hump, purplish-pink stretch marks, thinning skin or bruises. One of the main signs which will be used to make a diagnosis is a measurement of cortisol levels in the body. A diagnosis may only be made after several appointments and tests.
Lab tests for Cushing's Syndrome
Laboratory tests which are likely to be recommended in order to detect cortisol levels include (1):
- 24-hour urinary free cortisol test: A urine sample will be requested several times a day for measuring the amount of cortisol in the body over a 24-hour period.
- Dexamethasone suppression test: A low-dose steroid, dexamethasone (a synthetic glucocorticoid in pill form) will be given, to be taken orally every 6 hours for a test period of 4 days. Low doses will be given for the first 2 days, and will be increased during the remaining 2 days. A urine sample will be taken 24-hours before the medication is taken, and on every day of the test as well. Blood samples will also be requested and sent to a laboratory for assessment to check how much of the hormone the body produces. Normally, cortisol levels in the blood and urine will drop when taking the medication as both the hormone and drug will signal the pituitary gland to reduce the secretion of ACTH (adrenocorticotropic hormone). A doctor will also carefully assess results against other factors which can alter them, such as alcoholism, depression, elevated oestrogen levels, stress or another acute illness. Certain medications may also need to be ceased at least a week before this test as they too can influence the results.
- Late-night salivary cortisol levels: Cortisol is measured in the saliva from a sample taken during the night. Normally, cortisol levels will drop significantly during the night. If levels are high, it may indicate a cortisol production problem for further testing. A midnight plasma cortisol test may also be done and blood samples analysed in the laboratory for the same purpose.
If cortisol levels are in excess following these tests, a doctor may recommend a consultation with hormone disorder specialist (endocrinologist).
An endocrinologist may begin testing to find the cause of increased cortisol in the body, either through stimulating or suppressing the body with hormone medications. Tests may include:
- CRH (corticotropin-releasing hormone) stimulation test: This test will assess the pituitary gland for any potential tumours which could cause elevated cortisol levels. The test is sometimes done in combination with an inferior petrosal sinus sampling test (IPSS), which also assesses the function of the pituitary gland and whether the correct hormones are being produced. A blood sample is taken from the petrosal sinuses (i.e. the veins which normally drain the pituitary glands) and from a vein in the forearm. For both tests, a catheter (thin tube) is used to extract blood from the sinuses surrounding the pituitary gland, as well as from a vein in the arm, after a dose of CRH is administered. The results of the two samples from each test will be analysed against one another. High levels of ACTH and cortisol may indicate a tumour on the pituitary gland, especially if the levels are higher in the sinus sample. Similar results from both the sinus and forearm samples may indicate that the root cause of the problem does not stem from the pituitary gland itself. Levels which are not elevated may then prompt a doctor to look for a potential tumour of the adrenal glands.
- Imaging tests (radiologic imaging): A doctor may also recommend tests which allow for highly detailed visuals of the pituitary and / or adrenal glands in order to detect possible abnormalities. Tests which can provide this include MRI (magnetic resonance imaging) or CT (computerised tomography) scans. Other imaging tests may be done with X-rays of the pituitary and adrenal glands to assess for abnormalities, such as tumours, as well as the size and shape of the glands too. Imaging procedures will not necessarily be used to make a diagnosis for Cushing’s syndrome, but rather to determine abnormalities which may be at the root cause of symptoms. Sometimes benign tumours exist but do not produce detrimental symptoms.
Cushing's syndrome treatment
Once an excess of cortisol in the body has been diagnosed, as well as the possible causes of this distinguished during testing, a diagnosis can be made and appropriate treatment administered. Treatment for Cushing’s syndrome is very much dependent on the cause of elevated cortisol levels. The primary focus of treatment is to lower levels of the hormone in the body to that of a normal state, and thereby alleviate damaging symptoms.
Options available to a doctor to use as treatment methods include:
- The reduction or cessation of corticosteroid use: Often, Cushing’s syndrome develops as a ‘side-effect’ of treating another illness with corticosteroid medications. A doctor will assess the current dosage being taken, and the illness it is being used to treat and make an adjustment that takes benefits and risks into careful consideration. Any corticosteroid medication must never be reduced or ceased altogether without the express direction of the treating doctor. Any adjustments (tapering) must be supervised by a medical doctor so as to avoid a deficiency in cortisol levels. A doctor can either control symptoms of Cushing's syndrome by reducing the dosage of the treating medication for a set period of time, while still adequately treating the other illness, or prescribe non-corticosteroid medications (allowing for the corticosteroid medication to be given in reduced doses or ceased altogether).
- Surgical procedures: If a tumour is identified as being the cause of the condition, one may be referred to a surgical specialist. A neurosurgeon is likely to be recommended for the surgical removal of pituitary gland tumours, often performed through incisions made in the nose (nostril) and / or upper lip (transsphenoidal adenomectomy). The procedure is an extremely delicate one and may achieve an 80% success rate (at least) if a surgeon has extensive experience. Surgery can be repeated if results are temporary, much improving symptoms. Tumours of the adrenal glands (lungs or pancreas) may also be surgically removed (bilateral adrenalectomy), although these procedures are performed using minimally invasive techniques (smaller incisions over the abdomen or along the sides of the body – laparoscopic techniques). Following any surgical procedure, a doctor will likely recommend taking a cortisol replacement medication during the healing process, encouraging the correct amount to be produced and circulated in the body. Most can cease the taking of this medication within a year. Adrenal hormone production is normally restored following surgery, but this can be a slow process (taking up to a year or longer) and medications may be successfully tapered thereafter. Few cases require lifelong medication following surgery, this is usually only necessary if adrenal function fails to fully return to normal.
- Radiation therapy: The surgical removal of tumours may not be totally possible. Radiation therapy may be recommended for those who are not suitable candidates for surgery (for medical reasons) or in conjunction with a surgical procedure. Radiation treatment is typically given in small doses over a period of 6 weeks, and alone can achieve symptom improvements of at least 40 to 50% in adults and up to 80% in children. Alternatively, Gamma knife surgery or stereotactic radiosurgery can be used where a large dose of radiation is delivered as a single treatment, thereby reducing radiation exposure to tissues surrounding the tumour. Medications may also be used in conjunction with radiation treatment which can help to speed up recovery. Sometimes chemotherapy may be a recommended form of treatment instead.
- Medications: For those who are either not suitable candidates for surgery or radiation treatment, or where these treatments have not proven successful, medications may be prescribed to control the production of cortisol. Severe cases of Cushing’s syndrome may also be treated with medications prior to a surgical procedure as a way to minimise risk. Medications prescribed either function as a target for ceasing cortisol production in the adrenal glands, decreasing the production of ACTH in the pituitary gland or blocking the effects of cortisol on tissues if glucose intolerance or type 2 diabetes is also present. Medication side-effects can include nausea and vomiting, headaches, fatigue, muscle aches, swelling, low potassium levels, elevated blood pressure or liver toxicity (in severe instances). Hormone replacement medications may be recommended in some instances where it is found that other hormones normally produced by the pituitary or adrenal glands become deficient due to the taking of drugs for the treatment of Cushing’s syndrome.
For many who have undergone surgical treatment, post-op recovery can take between two and three weeks before one is able to return to normal daily activity.
It is normal to experience nasal congestion, sinus headaches and fatigue during the initial stages of recovery as cortisol levels decline following treatment. Any adverse ailments and symptoms gradually reduce in intensity as the body heals. Medication supplements may likely be recommended for between 6 and 18 months, especially after surgical treatment.
A doctor will request periodic check-ups to monitor overall state of health and track progress being made in returning to normal function. To do this, a doctor will request blood samples to test cortisol levels. Cortisol measurements are usually taken 1 to 2 weeks following surgery.
Almost all symptoms of Cushing’s syndrome are reversible, but take a considerable amount of time to achieve. Many can expect symptoms to subside within 1 to 2 years following surgical treatment.
Common complications of Cushing's Syndrome
Cushing’s syndrome must be medically treated. If not, the condition can result in any of the following complications:
- Loss of muscle mass and lack of muscle strength (due to weakness)
- Osteoporosis / bone loss (due to weakening), and resulting in an increased risk for fractures (ribs and bones in the feet)
- Type 2 diabetes
- Hypertension
- More frequent and difficult to treat infections
- Kidney stones
- Pituitary tumour enlargement
- Interference with the production of other hormones in the body (due to pituitary tumours)
Some complications can develop following surgical treatment. These include:
- Surgical risks which include bleeding, infection or adverse reactions to anaesthetic.
- Abnormally low levels of cortisol (which can be rectified with hydrocortisone replacement medications while recovering from surgery) following the removal of a pituitary or adrenal tumour.
- Permanent loss of the ability to produce cortisol if both adrenal glands are removed (treatment will involve long-term replacement cortisol medications).
- Inability of the pituitary glands to produce other necessary hormones for the body’s normal function following large tumour removal. These include thyroid hormones, growth hormones, oestrogen, testosterone and vasopressin. Self-administered injections or synthetic hormone medications will need to be taken to correct this.
- General hormone function disruption due to radiotherapy.
- The possible development of a complication known as Nelson’s syndrome (although rare) in instances where both adrenal glands are removed. In this condition, a tumour develops rapidly inside the pituitary gland causing vision loss or double vision, headaches and darkening of the skin. The tumour will need to be surgically removed, and possibly treated further with radiotherapy.
Reference:
1. National Institute of Diabetes and Digestive and Kidney Diseases. April 2012. Cushing's Syndrome: https://www.niddk.nih.gov/health-information/endocrine-diseases/cushings-syndrome [Accessed 08.08.2017]