- Endometriosis
- What are the stages of endometriosis?
- What are the symptoms of endometriosis?
- What are the risk factors and complications of endometriosis?
- How is endometriosis diagnosed?
- How is endometriosis treated?
- How to cope with endometriosis and the outlook of the condition
- FAQ about endometriosis
What is endometriosis?
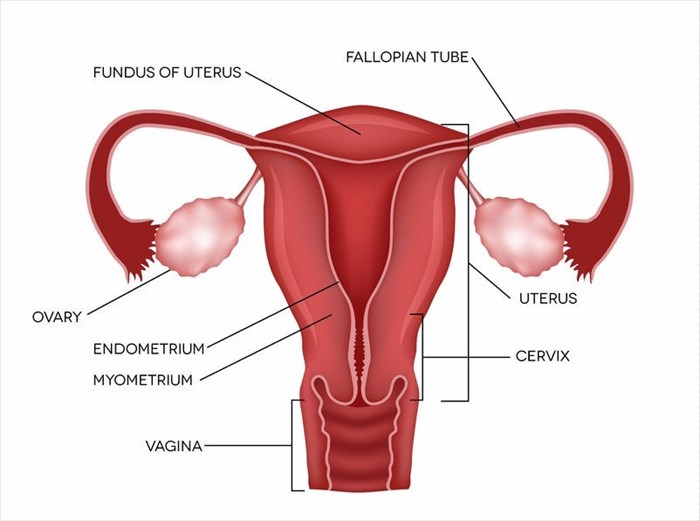
Pronounced “en-doe-me-tree-O-sis”, this can be a painful condition as it involves the endometrial tissue usually found in the endometrial lining, which is inside your uterus, developing outside of it instead, which can result in a number of complications.
The inside of your uterus is known as the endometrium. Each month you shed endometrial tissue from your endometrium during your menstrual cycle, this is known as menstruation or your period. The areas most commonly affected by endometriosis are the fallopian tubes, ovaries and the tissue that lines the pelvis. In some rare cases, endometrial tissue can sometimes spread to areas beyond the pelvic organs.
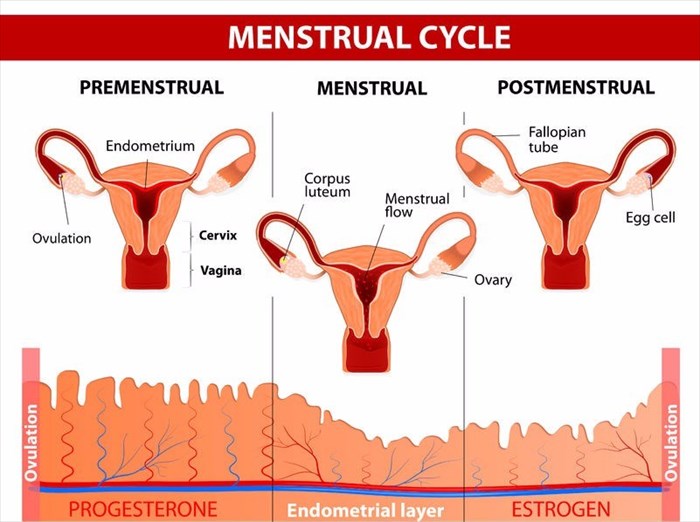
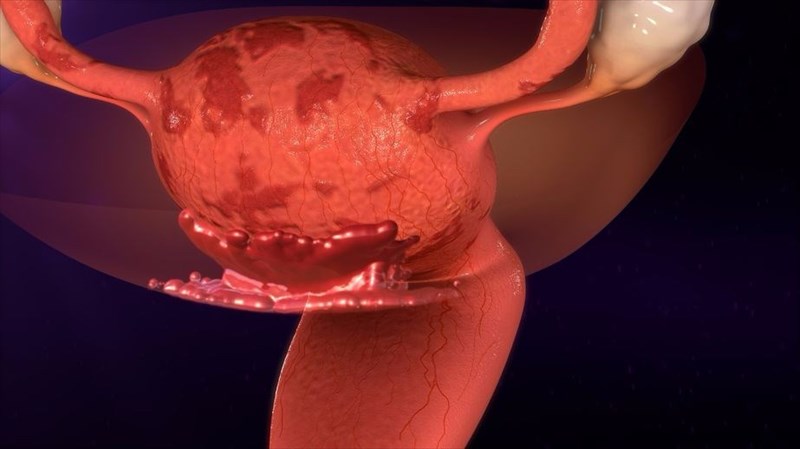
When you have endometriosis, the endometrial tissue that is displaced will continue to perform the way it should, thickening in preparation for a fertilised egg and then breaking down resulting in bleeding if the egg is not fertilised and you then have your menstrual cycle. However, because the endometrial tissue is displaced, it has no way to leave the body and therefore becomes trapped. When the ovaries are involved in the condition, then endometriomas, which are cysts, may form. The surrounding tissue can become irritated and inflamed, eventually resulting in the development of adhesions and scar tissue. Adhesions are abnormal groupings of fibrous tissue that may result in pelvic organs and tissues sticking to one another.
Endometriosis often results in pain, which can sometimes be severe, particularly during the sufferer’s menstrual cycle. Issues often arise where fertility is concerned, fortunately, there are a number of treatment options available.
How does endometriosis cause issues with my menstrual cycle?
The tissue that lines your uterus is known as endometrium, as mentioned above. Your body will release certain hormones every month that result in your endometrium thickening as it gets ready for the implantation of a fertilised egg and pregnancy (i.e. a sperm cell has fertilised an egg released from your ovary and this attaches to the uterine wall in order to develop). If you do not fall pregnant, the endometrium will shed, this is when you get your period.
If you suffer from endometriosis, the tissue that implants itself on the outside of your uterus will act as though it is still located within the lining of the uterus. This means that when you have your menstrual cycle, the tissue will thicken and shed which will result in bleeding. However, this shedding has nowhere to go to escape the body as is the case in a normal menstrual cycle. Thus, the tissue implants and becomes irritated and often painful. As stated earlier, this can then form scar tissue or cysts (fluid-filled sacs) in some cases. The scar tissue is what makes it difficult for some endometriosis sufferers to fall pregnant.
Other Articles of Interest

In Vitro Fertilisation (IVF)
We’ve all heard the term ‘test-tube babies’ – something that’s been linked with fertility treatment procedures, especially in vitro fertilisation (IVF), for many years. What does it all entail?

Egg Freezing
Should I freeze my eggs? It's a big question. Making this kind of decision can quickly become overwhelming. We simplify the process so that you can make the most informed decision...

Ultrasound scan
What is an ultrasound scan and how does it work? We look at the numerous ways this screening and monitoring tool is used in medicine today. Here's everything you need to know before having one...