Defining hepatitis
What is hepatitis?
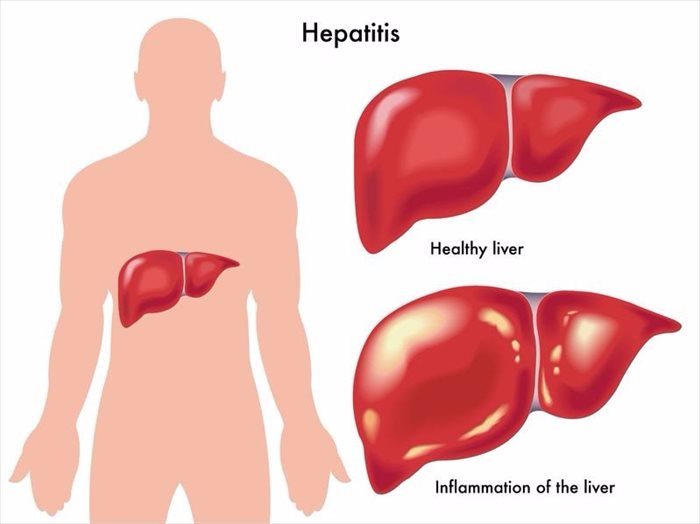
Hepatitis is inflammation of the liver, and has various underlying causes. Inflammation can worsen, and develop into more severe conditions such as cirrhosis (irreversible scarring of the liver), fibrosis (a thickening and scarring of liver tissue) or liver cancer.
Viral infections are the more common culprits causing hepatitis, but inflammation can also be brought on as a side-effect of illicit drug use, medications, excessive alcohol consumption and various toxins (known as toxic hepatitis). Typically, toxic hepatitis resolves itself when the underlying cause is removed. Complications will, however, depend on the nature of damage caused to the liver. When the body produces antibodies that work against the normal function of the liver, another cause can result in autoimmune hepatitis.
How does the liver function?
The liver is an essential organ for overall well-being and is located on the right upper quadrant of a person’s abdomen. The liver regulates the body’s metabolism levels which is vital for our overall health.
Some of the critical functions of the liver include filtering out toxins (and bilirubin, cholesterol and hormones) in the body, aiding bile production for comfortable digestion, metabolising proteins, carbohydrates and fats, activating enzymes, synthesising plasma, storing minerals, vitamins and glycogen, as well as the synthesis of clotting factors and hormones.
Other Articles of Interest

Liver Disease / Hepatic Disease
The liver is a phenomenal organ with the ability to heal itself. However, in some cases, the constant damage and abuse to it can cause liver disease and even liver failure.

Addictions
Addiction is defined as a chronic dysfunction in the brain that typically involves motivation, memory and reward. What are the most common types of addiction and how do you recognise the signs?

Liver Cirrhosis
Severe scarring of the liver, often as a result of long-term exposure to toxic causes, leads to irreversible damage. Here's how to recognise the signs of liver cirrhosis...