In order to diagnose irritable bowel syndrom (IBS), a doctor will need to take a full personal and family medical history and also assess the sufferer through a physical examination.
The following explains the diagnosis process in detail:
Criteria needed to make an accurate diagnosis of IBS
Due to the fact that symptoms vary from one IBS sufferer to another, there is no definitive list that allows for a concrete IBS diagnosis. Diarrhoea, constipation and abdominal discomfort can often be standalone conditions or associated with other diseases. Thus making an irritable bowel syndrom diagnosis often involves the process of elimination that rules out other conditions as the underlying cause of the symptoms present.
To aid in this process, doctors and researchers have created a method that consists of two steps or rather, two sets of criteria in order to diagnose IBS and other gastrointestinal disorders, known as functional gastrointestinal conditions in which the bowel does not function normally.
These criteria are both based on the symptoms the person is experiencing after all other conditions have been ruled out. The criteria are as follows:
- Manning criteria – This set of criteria focuses on the pain, incomplete bowel movements, changes in the consistency of the stool, the presence of mucus in stools, as well as the pain that is relieved through defecation. The more of these symptoms that are present, the higher the likelihood of the diagnosis being IBS.
- Rome criteria – This set of criteria determines specific symptoms and signs that must be present before the diagnosis of IBS is possible. The important signs are discomfort or abdominal pain that lasts for a minimum of three days of the month, experienced over the most recent three months. This must be associated with at least two of the following:
- Improvement of discomfort or pain through defecation
- Inconsistency of stool
A doctor will assess the degree to which the above criteria apply to the person being diagnosed and will also look into any other signs or symptoms that may indicate a more severe condition. There are a few red flag symptoms and signs that may require additional testing to be conducted.
These red flags are:
- Weight loss
- Bleeding of the rectum or blood in the stool.
- Fever
- Experiencing abdominal pain that does not subside through a bowel movement or if it occurs at night.
- Chronic diarrhoea, especially if it keeps you awake at night.
- Anaemia that is linked to an iron deficiency.
If however, the person being diagnosed fits the criteria for IBS, then adoctor may recommend a treatment course without the need for more tests. If the person does not respond to the suggested treatment, the doctor will then conduct additional testing.
IBS tests
Tests used in the diagnosis of irritable bowel syndrome often include stool studies to examine the stool for infection or possible issues with the intestine's ability to absorb nutrients from food, this is known as malabsorption.
Additional tests may involve undergoing several tests to rule out any other causes resulting in IBS symptoms. These usually involve laboratory tests - which typically include routine tests to monitor one's health for conditions and diseases and determine treatment, and imaging tests – these let doctors take a look inside the body through monitoring and examining the forms of energy patterns created by the body tissues that create an image for doctors to examine (e.g. an X-ray).
These are explained accordingly:
Lab tests
- Blood tests – IBS symptoms are similar to those of celiac disease which is a food sensitivity to rye, barley and wheat. Blood tests are conducted in order to rule this disorder out. It is vital to note that if children have IBS, their chances of developing celiac disease is far greater than children who do not have IBS. An upper endoscopy is often performed should a doctor suspect that a person has celiac disease. This procedure is done to obtain a biopsy (wherein tissue is removed in order to examine the body for disease) from the small intestine.
- Tests for lactose intolerance – The enzyme that is needed in order to digest and absorb the sugar found in dairy products is known as lactase. If this enzyme is not produced by the body, a person may experience problems similar to those that are caused by IBS. These include gas, diarrhoea and abdominal pain. To determine if lactose intolerance is the cause of the above symptoms, a breath test may be conducted by a doctor, he/she may also recommend eliminating dairy products for a few weeks in order to determine if a lactose intolerance is the cause of IBS-related symptoms. If the symptoms resolve after avoiding dairy products, the diagnosis is lactose intolerance, otherwise, further testing is done to possibly diagnose IBS.
- Breath tests – A breath test is performed in order to look for bacterial overgrowth. This is done by asking the person being examined to swallow a pill containing urea that is marked with a rare carbon isotope. After half an hour or so the person will exhale into a collection card for a few minutes, which will then be tested for the presence of H.Pylori bacteria. Bacterial overgrowth occurs when this bacteria infects the colon moves up and grows in the small intestine, this leads to the sufferer being bloated, experiencing abdominal pain or discomfort and diarrhoea. This tends to be a common condition in those have undergone bowel surgery, have a disease that results in the digestion process slowing down or those suffering from diabetes.
There are 3 types of breath tests:
- Hydrogen breath test (HBT) - Measures both the methane and hydrogen production of the digestive system. It does this in order to evaluate if there is a malabsorption of carbohydrates (dietary sugars). Secondly, the test determines if there is bacterial overgrowth in the small intestine that may be causing the abdominal pain.
- Bile acid breath test - The bile acids in the liver help digest the fats, also known as lipids found in the small intestine. If bacterial overgrowth is present, this process is affected. This kind of breath test makes use of a bile salt that has a radioactive tracer attached in order to assess if there is a bile salt dysfunction present.
- Xylose breath test - This is a highly specific and extremely sensitive test that tests the bacterial overgrowth in the small intestine.
- Stool tests – The stool is often examined for parasites and bacteria if a person is experiencing diarrhoea.
Imaging tests for IBS
- Radiography (X-ray) – X-rays, which are digital images produced through beams that are absorbed by different bodily tissue, are often used to obtain an image of the colon in order to detect any issues or areas of concern.
- Lower gastrointestinal (GI) series – This is a test where a doctor fills the large intestine through the rectum with barium (a liquid) that makes it easier to detect any issues in the human colon (large intestine) in an X-ray.
- CT (computerised tomography) scan – These scans create X-ray images of the internal organs that are cross-sectional (taken from different angles). When CT scans are conducted of the pelvis and abdomen, this helps a doctor to rule out any other conditions that may be the cause of the symptoms experienced, particularly if abdominal pain is one of them.
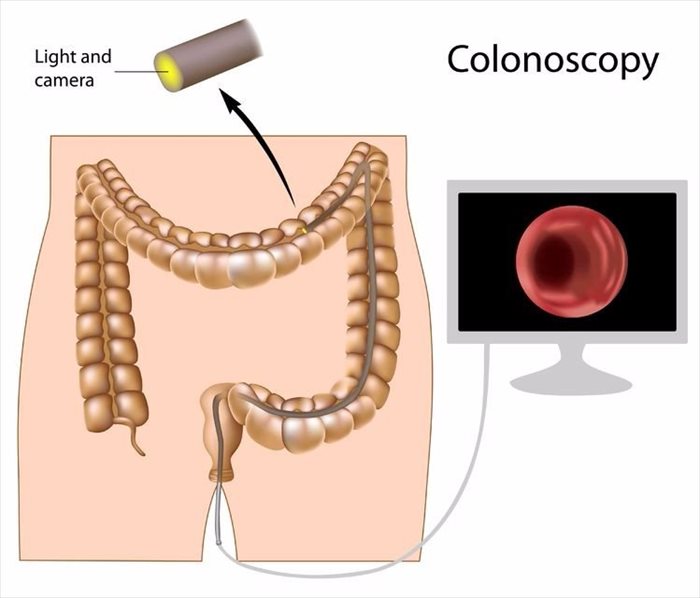
- Colonoscopy – In those suffering from chronic (ongoing) abdominal pain, who are over the age of 50 and experience symptoms that may be the result of a severe condition, a doctor is likely to perform a colonoscopy which is a diagnostic test that uses a small, flexible tube inserted via the anus in order to examine the entire length of the colon and its lining. This procedure is able to find ulcers, bleeding, tumours and more.
- Flexible sigmoidoscopy – This procedure allows for a doctor to take a closer look at your sigmoid (lower colon) and rectum. The lighted, flexible tube-like instrument, known as a sigmoidoscope is inserted into the rectum in a gentle fashion and then passed into the lower colon.