- Liver Disease / Hepatic Disease
- What are the causes/types of liver disease?
- What are the stages of liver disease from initial inflammation to liver failure?
- What are the symptoms and risk factors of liver disease?
- What is the diagnosis, treatment and prevention of liver disease?
- The liver disease diet and outlook
What is the diagnosis, treatment and prevention of liver disease?
How is liver disease diagnosed?
In order for the doctor to find the exact cause, as well as the extent of the damage done to the liver, both of which are vital factors as these, will guide the treatment plan, he or she is likely to begin with running through a complete health history of the patient as well as a physical examination.
Once this has been completed, the doctor is likely to recommend the following:
- Blood tests – Blood tests conducted when the liver is concerned are known as liver function tests and are able to diagnose the presence of liver disease. A number of other blood tests are also able to detect any other liver issues as well as genetic disorders and conditions.
- Imaging/screening tests – The doctor may conduct an MRI (magnetic resonance imaging) which is a scan that uses radio waves and magnetic fields in order for detailed visuals to be made of the liver. A CT (computed tomography) scan may also be conducted which uses specialised X-ray devices to create cross-sectional visuals of the liver.
- Biopsies (tissue analysis) – A biopsy involves the removal of a sample of tissue taken from the liver in order for it to be examined. This kind of biopsy is done while the patient under local anaesthetic while the doctor inserts a long and thin needle into the skin and into the liver to obtain a sample which will be sent to the lab for analysis.
How is liver disease treated?
The diverse types of liver diseases will each have their own treatment regimen that is specific to the disorder. For example, in the treatment of hepatitis A, the plan will need to include supportive care in order for hydration to be maintained while the patient’s body fights off and resolves the infection. Those who suffer from gallstones may need to have surgery done to remove their gallbladder. Other conditions may require more long-term treatment in order for the infections to be controlled and the complications reduced.
Patients who have cirrhosis or the end stages of liver disease may need medications to aid in controlling protein absorption in their diet. Proteins create waste products through their process of absorption, when the liver is cirrhosed, its ability to metabolise and process waste products is hindered, this results in ammonia levels in the blood being elevated which causes confusion, lethargy and the potential for the patient to slip into a coma, this is known as encephalopathy. Water pills, known as diuretics and a low-sodium (salt) diet may be needed in order to reduce a person’s water retention resulting from the excess fluid being trapped in the body’s tissues.
For patients who have a large amount of fluid that has accumulated in their abdominal cavity (i.e. ascites fluid), this fluid can sometimes be removed through the use of paracentesis. This method uses a hollow needle or a catheter that is inserted into the abdominal cavity (peritoneum) to remove the excess fluid. This is done while the patient is under local anaesthetic. This fluid is also able to become infected, therefore a paracentesis can also be used to detect any infection.
**Just to recap on ascites:
- Ascites – Pronounced “ah-SIGH-tees”, this condition refers to the build-up of fluids, specifically the fluid containing protein known as ascetic, in the abdominal cavity (peritoneum) due to an increase in blood pressure of the blood vessels in the liver forcing fluid to accumulate in the belly.
In cases of portal hypertension (high blood pressure), operations are sometimes performed in order to minimise the patient’s risk of internal bleeding. These methods often include a blood transfusion combined with medication to reduce the blood pressure.
The final treatment option is for those who suffer from liver failure to receive a liver transplant. This is a surgical procedure wherein the infected liver is removed and replaced with a healthy liver from a donor.
Can liver disease be prevented?
The majority of cases of liver disease can be prevented. Roughly 5% of liver disease deaths are as a result of genetic and autoimmune disorders, with more than 90% being due to the three main risk factors.
These risk factors are:
- Viral hepatitis – This is a highly contagious condition and is a result of a hepatitis A infection.
- Obesity – This is the leading cause of fatty liver disease which is the most common type of liver disease. Obesity can lead to the accumulation of fat in the liver which causes strain and damage.
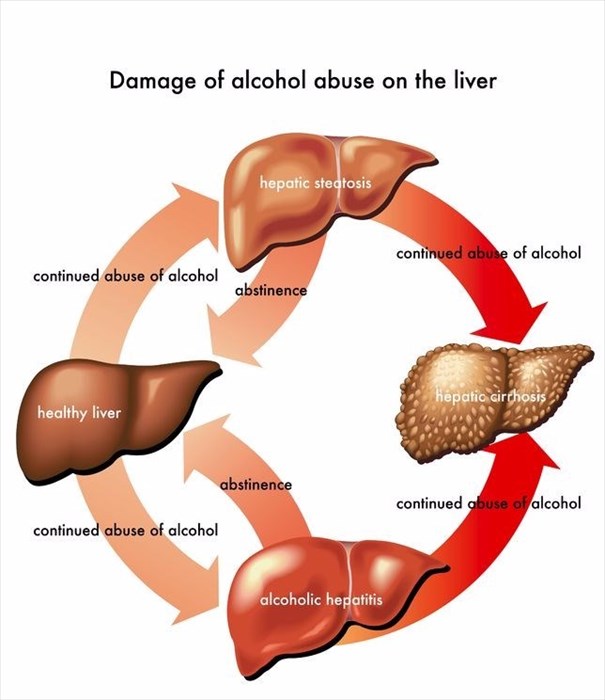
- Alcohol – A number of cases of fatty liver disease will progress to alcoholic hepatitis amongst heavy drinkers, and eventually to alcoholic cirrhosis. Alcohol contains a number of toxins that are harmful to several organs in the body. The liver has to process these toxins which can damage the liver cells and result in inflammation. The prognosis of this condition, as with most liver diseases, will depend on the severity of the damage done.
The following are factors that are able to significantly reduce liver disease developing:
- Not drinking alcohol in excessive amounts – For normal adults, an acceptable amount of alcohol use is one unit a day for women and elderly men (over 65 years old), and healthy men younger than 65 can have as many as two units a day. For drinking to be classified as high-risk or heavy, this means that a person consumes more than a total of three drinks a day, for women and elderly men, this means to more than seven drinks in total over a period of a week and for younger men this will be more than 14 drinks per week. If you think you may suffer from alcoholism, then speak to your doctor about a rehabilitation program.
- Avoiding dangerous behaviour – Using drugs intravenously or sharing needles is considered risky behaviour and will significantly increase one’s chances of contracting an infection that may lead to liver disease. This also includes having unprotected sex.
- Using medications with care – Taking drugs, whether prescription or over-the-counter should be done with care and within the recommended dosage. Medications should not be mixed with alcohol.
- Getting vaccinated – There are vaccines available for hepatitis (A and B). These will help control the risk of infections that cause liver disease for those who are most likely to contract these infections.
- Maintaining a healthy diet and weight – Non-alcoholic fatty liver disease can often stem from obesity. This disease can be prevented through controlling one’s weight through a proper exercise regime and nutritional diet.
- Avoiding contact with someone else’s blood and their bodily fluids - The hepatitis viruses are easily spread and often in areas where sanitation and hygiene is poor.