How will signs of a stroke be treated?
When a person is brought in to a medical facility with stroke-like symptoms, a flurry of activity can be expected. Being an emergency situation, specialists will be swiftly notified for appropriate diagnosis and testing, before any treatment can be effectively administered.
A neurologist (specialist of nervous system disorders) will be called to assess the person, confirm symptoms of stroke and also identify the type of stroke (depending on the parts of the body affected or showing the clinical signs of the stroke) and also the extent of damage caused to the person already. No effective treatment can really be implemented until all of this has been established by medical professionals.
If immediate inappropriate treatment is administered before medical staff are certain of what they are dealing with, further damage to the brain and nervous system can occur. It is imperative that appropriate emergency care is given.
In the moments following arrival at a medical facility (hospital), medical staff will examine the person. If possible and the person is able to liaise with medical professionals, a medical history will be discussed. Doctors and nurses will promptly begin checking blood vessels in the eyes (using an ophthalmoscope to see if there are any cholesterol crystal or clots at the back of the eyes), measuring blood pressure and pulse rate, as well as listening for abnormal sounds in the heart and prominent carotid arteries in the neck to assess any blockage of blood flow to the brain using a stethoscope.
Medical staff will be looking for any indication that a blockage of the arteries is perhaps an underlying cause (this is done by listening for a bruit or ‘whooshing’ sound), as well as other physical signs of stroke (such as balance problems, poor coordination, body weakness, confusion, vision problems and numbness or paralysis in the face, arms and legs).
If you are having a stroke and are able to communicate, the emergency team will also try and talk to you about your symptoms, determine any medications or supplements you may currently be taking, assess if you have recently experienced any head injuries, as well as try and gain some family medical history.
If any signs during the initial emergency assessment are clear indications of a possible stroke, medical professionals will then need to determine what specifically has caused it, where in the brain damage has been caused, and whether there is any bleeding in the brain. If you are unable to communicate, the team will see if perhaps a close relative or someone who knows you particularly well is available at the hospital to assist.
What tests are involved in diagnosing a stroke?
Tests will be necessary, not only to confirm a diagnosis of stroke, what type has occurred and the severity of damage for treatment, but also to try and rule out any other potential causes of the symptoms being experienced. This is critical. It could come down to an adverse reaction to a medication that was being taken at the time or even a brain tumour.
Tests which are likely to take place in the emergency room include:
- CT (Computerised tomography) scan: This imaging test combines a series of detailed X-rays using computer processing, from a variety of different angles to create cross-sectional visuals of bones, soft tissues and blood vessels in the body. A dye will be injected into the bloodstream to help create clear and detailed images of the neck and brain. This test will show exactly where in the brain bleeding is occurring (if haemorrhagic) or if an ischemic stroke has occurred.
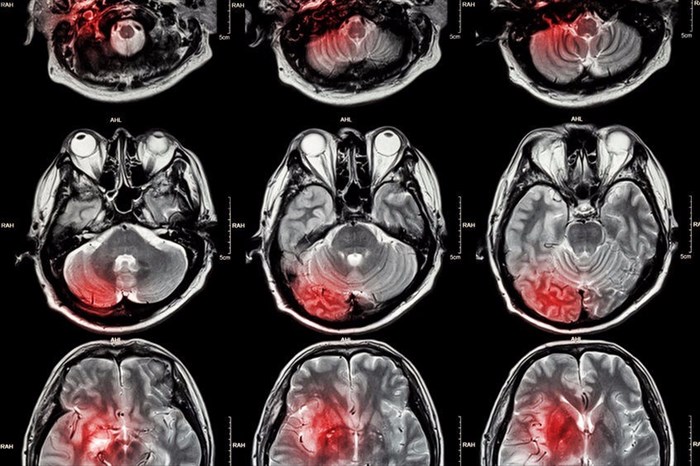
- MRI (Magnetic Resonance Imaging): Another imaging test which provides detailed images of the inside of the body is an MRI scan which uses strong magnetic fields and radio waves. This scan can also be used to determine the occurrence of a stroke, and its type. A doctor may inject a dye into a blood vessels to create clear and detailed images of arteries and veins, so as to determine the nature of blood flow in the body.
- ECG / EKG (Electrocardiogram): This test will be used to assess any potential heart abnormalities and possibly detect an underlying cause (especially those associated with an ischemic stroke). The test effectively records any electrical activity in the heart by measuring its rhythm and recording the speed at which it is beating.
- Blood tests: These can include a CBC (complete blood count), electrolytes, blood sugar level measurement, liver and kidney function, as well as a prothrombin time and INR assessment (measurement taken to see how long it takes blood to clot). These tests will effectively assist the emergency team with making appropriate treatment choices so as not to cause any further damage to the body. Essentially, the medical team will be looking for abnormalities which will be tell-tale signs in the blood. These can include things like abnormally high or low blood sugar, signs of infection, if critical blood chemicals are imbalanced, and assessing the blood’s ability to clot.
Emergency treatment may be followed by conducting the following tests (where necessary):
- If a doctor suspects that a stroke has occurred due to a narrowing of a carotid artery: Tests may include a cerebral angiogram (a thin, flexible tube is inserted through a small incision or cut and can be guided through major arteries – the carotid or vertebral arteries. A dye is injected to provide image clarity on an X-ray), carotid ultrasound (sound waves are used to created detailed images of the carotid arteries in the neck and may show the build-up of plaque and blood flow) or Doppler scan, MRA (magnetic resonance angiogram) or CT angiogram.
- If a doctor suspects that a stroke has occurred due to a heart abnormality: Tests may include a Holter monitoring, a telemetry test or echocardiogram (sound waves which create detailed images of the heart and help determine the presence of clots). A transoesophageal echocardiogram can also help a doctor determine the condition of the heart and potential presence of blood clots. A thin, flexible tube is inserted into the throat and down the oesophagus that connects the mouth and stomach. The close proximity of the oesophagus and heart allows a good view of potential abnormalities.
How will a stroke be treated?
Emergency treatment will effectively coincide with assessments and testing upon a patient’s arrival. If a person is unconscious or losing consciousness, the emergency team will prioritise difficulties with breathing in particular, and provide supplemental oxygen. Testing will be conducted on an emergency basis and as things are determined, treatment will be administered. Time is of the essence and can mean the difference between life and death in extreme instances, or that of severe disability and an easier recovery.
If an ischemic stroke type is determined, treatment will involve:
- Emergency medications: The first thing a medical team will wish to do will be to restore blood flow to the brain, alleviating clot damage. Treatment will involve medications that will begin to alleviate blood clot blockages as soon as possible (within 3 hours of the onset of stroke symptoms). Emergency medication may include aspirin (this helps reduce the likelihood of having another stroke by thinning the blood and preventing new blood clots from forming), a TPA (tissue plasminogen activator administered through a vein to dissolve blood clots within 30 to 60 minutes).
- Emergency procedures: Blood clots may require emergency medication treatment administered directly to the brain. This may involve a long, thin tube (or catheter) inserted through an artery (usually in the groin) which is then threaded to the brain to deliver thrombolytic medication in the precise area requiring treatment. Another procedure used to treat blood clots is a mechanical clot removal procedure (known as a mechanical thrombectomy). This involves the insertion of a catheter with a tiny attachment that can be used to physically break off and remove a clot.
- Other procedures: A doctor may recommend a procedure to open up a narrowed artery, and thereby reduce the risk of another stroke. Options available will depend on the nature of the stroke a patient experienced. Some options available include a carotid endarterectomy (plaque from the carotid arteries is surgically removed through an incision in the neck), or angioplasty (an artery in the groin will provide access to carotid arteries where a balloon is used to try and expand a narrowed artery due to clots, after which a stent is inserted to support the opening).
If a haemorrhagic stroke type is determined, treatment will involve:
- Emergency care: If this type of stroke is determined, the primary goal is to control any bleeding that occurs in the brain. Emergency treatment will involve alleviating the pressure that bleeding will cause. Medications may be administered to prevent any blood clots, seizures or vasospasms (spasms of arteries that lead to the constriction of blood vessels and increased blood pressure known as vasoconstriction), as well as lower pressure in the brain. Once bleeding is under control, the emergency team will provide supportive care which allows the rest of the body to absorb blood and promote healing. If it is determined that a large area was affected by a rupture or aneurysm and bleeding, surgery may be necessary to remove excess blood and alleviate pressure.
- Surgical procedures: Damage caused by ruptures may require surgery whereby a doctor will repair blood vessel abnormalities. Some repair procedure options include surgical clipping (a tiny clamp is placed at the base of an aneurysm to restrict blood flow to it, preventing rupture), a coiling or endovascular embolization (a catheter is inserted into a groin artery and guided to the brain where detachable coils are placed into the aneurysm, effectively blocking blood flow and allowing blood to clot), a surgical AVM or arteriovenous malformation removal (smaller AVM’s can be removed if located in an accessible area in the brain and thereby reduce the risk of rupture and another stroke), an intracranial bypass (can be used to repair an aneurysm, complex vascular lesions or poor blood flow in affected areas of the brain), or stereotactic radiosurgery (this involves an advanced but minimally invasive procedure to treat vascular malformations using multiple beams of focussed radiation).
Stroke medications explained
One of the primary goals of any medication that is prescribed, especially during the emergency care stages, is to prevent another stroke from happening. The more damage that can be prevented the better.
Medications do depend on the type of stroke experienced and their specific underlying causes. Some medications work to break up existing blood clots or prevent new clots from forming. Others specifically target high blood pressure (hypertension) and cholesterol as a way to reduce the risk of blood flow blockages and narrowing of the blood vessels.
Some medication options may include:
- Anticoagulants: These medications interfere with the blood clotting process and purposefully prevent it from happening easily. Interference can also prevent any existing blood clots from becoming larger, and thereby causing pressure and distress in the body. These medications may be necessary once an ischemic stroke or TIA is identified as the type being experienced.
- Antiplatelet medications: A common medication used to promote blood thinning and prevent blood clots is aspirin. Sometimes aspirin is given in combination with other medications which work together to prevent blood from being able to accumulate / stick together, forming a clot. These medications are thus usually prescribed for those who have experienced an ischemic stroke. Medications are typically prescribed for an extended period of time as a means of prevention.
- TPAs (tissue plasminogen activators): This medication physically breaks up a blood clot and is commonly favoured during an emergency situation. It is administered intravenously (injected into a vein or artery). This way the medication can get to work quicker and break up blood clots that are causing distress associated with stroke. There is a risk of bleeding in the brain that, for some individuals, is too high a chance to take. Patients receiving this medication will be monitored with intense care.
- Blood pressure medications: During the initial physical examination upon arrival at a hospital, blood pressure will be measured and recorded. If blood pressure is too high, doctors may prescribe medications to lower it. High blood pressure aggravates symptoms of stroke and plays a key role in worsening the condition. High blood pressure can contribute to the breaking off of large chunks of plaque, which then help the formation of blood clots along. Beta-blockers, calcium channel blockers and angiotensin-converting enzyme inhibitors (ACE) are common medications which may be prescribed.
- Statins: These medications assist with lowering cholesterol levels as elevated cholesterol levels can also cause blockages when a build-up of plaque accumulates along the arterial walls. Prescribed medications work by blocking the enzyme in the body that typically helps to produce cholesterol (naturally). Blocking this enzyme effectively enforces the body to produce less of it and thereby reduces the risk of hyperlipidaemia (raised cholesterol). Preventing further build-up can contribute to prohibiting another stroke from occurring.