
What is Tramadol used for?
Tramadol has proved beneficial for those suffering ongoing (chronic) pain. The medication effectively works with the body’s central nervous system in order to relieve pain. Used for long-term treatment, this medication has been noted as potentially habit-forming, resulting in dependence in both a mental and physical capacity. Physical dependency can lead a variety of side-effects, especially when discontinued. The medication itself, is not classified as a narcotic, however. As dependency is a risk factor, Tramadol is classified as a controlled substance.
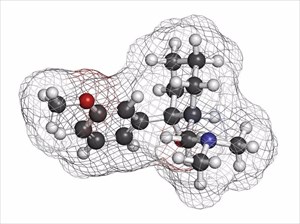
The medication is effectively a ‘centrally acting synthetic’ and works by inducing the release of serotonin in the brain, and inhibiting the reuptake of norepinephrine. This can create a ‘narcotic-like’ pain relief effect, which can lead to dependency. Serotonin and norepinephrine are the two chemicals in the brain directly linked with mood, as well as responsiveness to pain in the body.
The medication is mostly made up (about 80%) of ingredients inhibiting the reuptake of chemicals in the brain and the remaining 20% being pain-relieving components. The pain-reliving ingredients come from opioids, which are less likely than many other painkiller products to cause dependency. These include morphine, hydrocodone and oxycodone. Although a low percentage in terms of habit-forming content (opioids), the medication still carries a dependency risk for some individuals (this addiction usually develops through misuse).
Often, a doctor may consider Tramadol when other pain-relieving medications have not proved all that effective.
This medication is only available through prescription from a licensed medical practitioner in the following dosage forms (to be taken orally):
- Tablet (including disintegrating or extended-release forms)
- Suspension
- Capsule (extended-release)
Tramadol may be prescribed for a variety of medical conditions (not all of which are primarily associated with physical pain) that may respond favourably to the anti-inflammatory and non-steroidal effects of this drug, provided a medical doctor feels it appropriate.
The effects of both opioid and serotonergic ingredients can be effective for treating both the physical and psychological components of pain (in acute and chronic forms). These can include:
- Diabetic neuropathy: A diabetic person often experiences nerve damage in the body, mainly affecting their legs and feet. Nerve damage can cause considerable pain, as well as numbness. This can result in possible problems developing in the heart, blood vessels, digestive system and urinary tract. Symptoms of pain can range from mild to severe, and sometimes become life-threatening. Tramadol can be useful in managing chronic pain for those undergoing treatment for diabetes.
- Migraine: Migraine headaches that are accompanied by visual disturbances (known as migraine with aura) can be an intensely painful experience. Tramadol can provide effective relief for pain associated with this type of headache.
- Fibromyalgia: A chronic condition that is widespread in the body, pain levels vary in intensity throughout the musculoskeletal system. Some relief from pain and tender areas in the body can be achieved with this medication.
- Multiple Sclerosis (MS): An unpredictable and disabling condition whereby the immune system ‘attacks’ the protective sheath or covering of the body’s nerves, resulting symptoms of MS include pain and muscle spasms. Symptoms such as these can lead to problems with mobility. Treatment of multiple sclerosis with Tramadol can considerably alleviate moderate to severe discomfort.
- Anxiety, depression and obsessive-compulsive disorder (OCD): Those who suffer from constant symptoms of nervousness, worry, fear, hopelessness, apprehension and uneasiness can benefit from the chemical adjustments the taking of this medication can achieve. A medical doctor will prescribe this medication for these conditions with great care and consideration, especially if a person suffers from extreme forms of these disorders or displays addictive behaviours.
- Postherpetic neuralgia (pronounced post-hur-PET-ik noo-RAL-juh): This condition often develops as a complication of the Varicella Zoster virus (causing chickenpox and shingles). The condition is associated with damage to nerve fibres and the skin which can cause a burning pain.
- Reflex sympathetic dystrophy (RSD): Damage to the reflex sympathetic nervous system in the body can result in a burning-like pain (often described as a pain that feels like fire). Tramadol can help to alleviate this pain.
- Restless legs syndrome (RLS): A condition characterised by an uncontrollable urge to move legs, a sufferer often experiences ‘pins and needles’, itching and creepy crawly sensations which can be alleviated with Tramadol.
Other Articles of Interest

OCD (Obsessive-Compulsive Disorder)
OCD is different to being a perfectionist. It is a unique mental disorder. In this article, we unpack all you need to know about the condition...

Anxiety
Anxiety is a psychological, physiological, and behavioural state that may cause a sufferer intense distress. An anxiety disorder can be disabling, but it is manageable. Here's all you need to know...

Depression
Depression is more than just a case of the blues, we explore what the condition means and how to treat it...
