- Candida
- Causes of candidiasis
- Signs and symptoms of candidiasis
- Oropharyngeal / oesophageal candidiasis (oral thrush)
- Genital Candidiasis / vulvovaginal candidiasis (VVC) / Candidal vulvovaginitis
- Cutaneous Candidiasis / Candida Skin Infection
- Invasive candidiasis
- What is Candida die-off?
- Candida Diet and Outlook for the infection
Candida infection that involves the mouth, throat and/or oesophagus is referred to as oropharyngeal or oesophageal candidiasis or thrush.
Causes of oral thrush
Oral thrush occurs when certain medications (like antibiotics or corticosteroids) are taken or the immune system is weakened due to illness. These medications as well as certain health conditions disturb the natural balance of 'healthy bacteria' in the body which leads to the multiplication of Candida14. When this growth remains unchecked, an infection (candidiasis) occurs and leads to the development of various symptoms associated with oral thrush.
Oral thrush symptoms
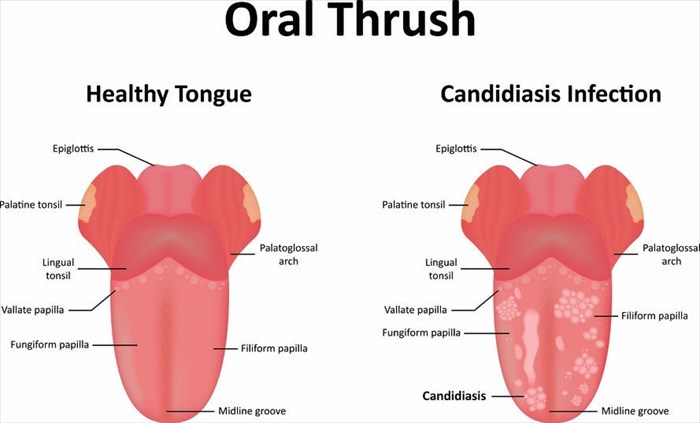
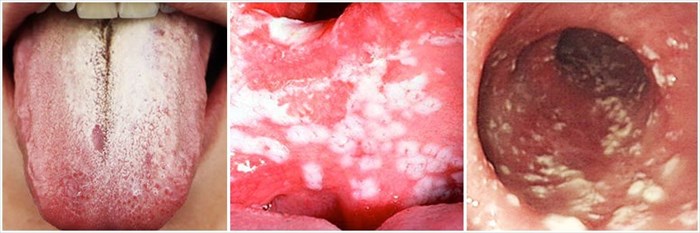
What does oral thrush look like?
Oral thrush is generally easily identified by a thick, white coating on the tongue and white patches / plaques on the insides of the cheeks and throat. As one descends down the throat and into the gastrointestinal tract (generally only visible when using an endoscope), the patches continue, as is evident in the images below.
Other symptoms may include:
- Soreness or redness in the areas affected
- Difficulty in swallowing
- Painful sores on the sides of the mouth that result in the corners cracking due to the build-up of microorganisms (this is known as angular cheilitis) – these sores often cause a burning sensation in the affected area
- Nausea
- Vomiting
- Weight loss
If you are experiencing any of these symptoms, it is advised that you see your doctor for treatment. The earlier treatment begins, the better the outlook.
Who is at risk of developing oral candidiasis?
Babies, toddlers, the elderly and people who suffer from a weakened immune system are most at risk of experiencing oral candidiasis (oral thrush). These infections are uncommon in healthy adults.
Other factors that are associated with the development of oesophageal and oral candidiasis, these include:
- Broad-spectrum antibiotic use – these are antibiotics that work against a large range of bacteria, including the healthy bacteria that keep Candida growth in check.
- Corticosteroid use (including inhaled corticosteroids for conditions like asthma)
- Diabetes that is poorly managed
- Poorly fitted dentures
- Cancer treatments – These include radiation and chemotherapy as these treatment methods have an adverse impact on the immune system
- HIV/AIDS infection
- Organ transplantation
Can oral candidiasis be prevented?
The development of oral thrush depends on the strength of one’s immune system, this is why babies, the elderly and the immunocompromised are often most affected. Practising good oral hygiene helps to prevent oral thrush from occurring.
Some studies show that mouthwash containing chlorhexidine (CHX) can aid in preventing oral thrush15,16. Those who use an inhaler for the administration of corticosteroids (asthma medication), can benefit from washing their mouth out with mouthwash or even water after using their inhaler.
Diagnosis of oral thrush
An oral thrush infection will be diagnosed based on visible symptoms. The treating doctor may also scrape off some of the affected area in order for it to be examined. This procedure is quick and painless and allows for the sample of the infected area to be analysed and tested for the presence of fungal infections.
A culture test using a cotton swab can also be performed, however, due to the fact that Candida organisms occur naturally in the mouth, if the culture test is positive, this is not enough evidence to make an accurate diagnosis of infection (candidiasis).
Treatment of oral thrush and outcome
Antifungal medication is typically prescribed for oral thrush16. The duration and type of treatment will be dependent on the infection’s severity, as well as various factors regarding the sufferer such as their age and immune system status.
Topical treatments including nystatin suspension and clotrimazole troches are often used in the treatment of oral thrush. Antifungal medication that is systemic (i.e. drugs that act through the entire body), such as itraconazole or fluconazole, are sometimes necessary when oropharyngeal infections do not respond to other medications.
Itraconazole or intravenous fluconazole are common treatments for Candida esophagitis. In more severe cases of oesophageal candidiasis that do not respond to antifungal medications, a treatment containing amphotericin B may be used. This form of treatment will injure the membranes of the fungal cell, making it more permeable for other medications to treat and eliminate.
References
14. Agrawal A, Singh A, Verma R, Murari A. Oral candidiasis: An overview. Journal of Oral and Maxillofacial Pathology. 2014;18(4):81. doi:10.4103/0973-029x.141325
15. Scheibler E, Garcia M, Medina da Silva R, Figueiredo M, Salum F, Cherubini K. Use of nystatin and chlorhexidine in oral medicine: Properties, indications and pitfalls with focus on geriatric patients. Gerodontology. 2017;34(3):291-298. doi:10.1111/ger.12278
16. Oral thrush: Prevention during cancer treatment. Ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK367590/. Published 2006. Accessed May 22, 2019.
17. Patil S, Rao R, Majumdar B, Anil S. Clinical Appearance of Oral Candida Infection and Therapeutic Strategies. Front Microbiol. 2015;6.doi:10.3389/fmicb.2015.01391