- Candida
- Causes of candidiasis
- Signs and symptoms of candidiasis
- Oropharyngeal / oesophageal candidiasis (oral thrush)
- Genital Candidiasis / vulvovaginal candidiasis (VVC) / Candidal vulvovaginitis
- Cutaneous Candidiasis / Candida Skin Infection
- Invasive candidiasis
- What is Candida die-off?
- Candida Diet and Outlook for the infection
Genital candidiasis, more commonly referred to as 'genital thrush' can affect both men and women. It is, however, more common in women and is responsible for the development of a vaginal yeast infection (aka vaginal thrush). In men, it generally affects the head of the penis and foreskin, and is known as balanitis.
What causes genital candidiasis?
The majority of Candida infections are a result of an imbalance in the individual’s own naturally occurring, healthy organisms. Candida yeasts generally reside on the skin, in the GI (gastrointestinal tract), mouth and vagina without resulting in any symptoms.
In the case of an imbalance occurring, the organisms will multiply and grow, causing and infection (candidiasis). Any change to the body's natural environment that disrupts this balance is a culprit in the development of this type of infection.
Who is at risk of developing genital candidiasis?
Roughly 75% of adult women around the globe have suffered from a yeast infection at least once in their lives18. On rarer occasions, men may also develop genital candidiasis. The condition tends to affect those who have a weakened immune system.
The following are risk factors for genital candidiasis for women and in more rare cases, men:
- Using broad-spectrum antibiotics for a long period of time
- Using corticosteroids
- Wearing tight underwear that is not cotton
- Wearing wet clothing near the genital region for a prolonged period of time
- Having a weakened immune system due to recent illness
- Having poorly managed diabetes
- Undergoing cancer treatments
- Having sexual intercourse with an infected person (this is rare)
Female only risk factors include:
- Being pregnant as this changes hormone levels in the body which alters bacterial balance in the vagina
- Taking birth control pills
- Using feminine hygiene sprays or douches
- Scratches occurring in the vagina due to the insertion of tampons or other objects
Genital thrush in women (vaginal thrush)
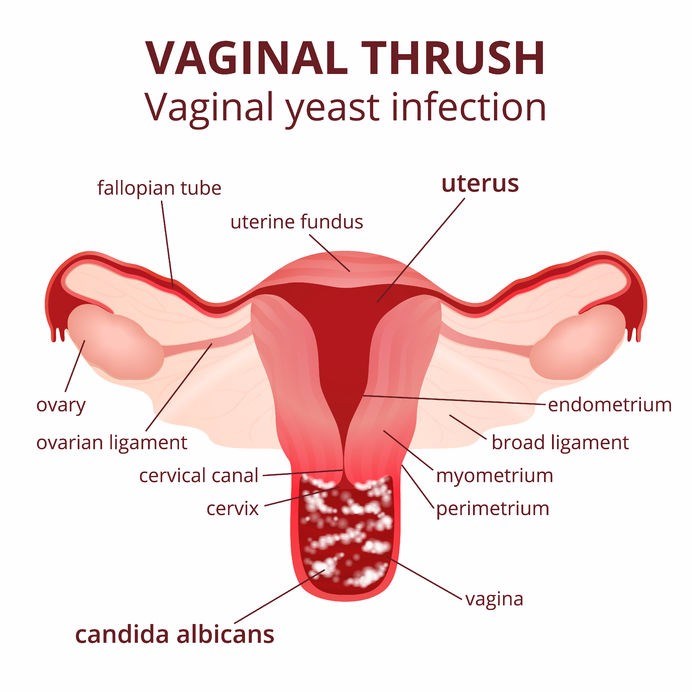
Vaginal thrush is a common occurrence when the imbalance of fungus occurs, for example, when the normal levels of acidity in the vagina change or when there is a hormonal imbalance. This causes Candida to multiply which can lead to candidiasis and the symptoms associated with the infection. This kind of Candida infection is caused by Candida albicans (C. Albicans).
Vaginal thrush symptoms
Women who have vaginal thrush will commonly suffer from:
- Genital burning and itching
- Increase in abnormal vaginal discharge that, in some cases looks similar to cottage cheese
- Pain or burning when urinating
- Discomfort during sexual intercourse
- Swelling and redness of the vulva and vagina
Genital thrush in men
Men can also get genital candidiasis, this often results in inflammation accompanied by an itchy rash forming on the head of the penis and foreskin and is known as fungal balanitis. This condition is more common in uncircumcised men.
Signs and symptoms of thrush in men (balanitis)
Signs and symptoms include:
- Moist areas of skin on the penis, sometimes accompanied by smelly, thick, white, cottage-cheese-like discharge which collects under the foreskin.
- Patches of shiny, white skin in the genital area
- Inflammation of the penis accompanied by redness, itching and burning sensations
- Difficulty retracting the foreskin
- Pain during urination
- Discomfort or pain during sexual intercourse
The symptoms of genital candidiasis in both sexes are very similar to a variety of other infections of the genitals. It is therefore vital that you make an appointment with your doctor should you have any of the above-mentioned symptoms.
Yeast infections are not typically spread or caused by sexual intercourse. However, it is estimated that less than 15% of men may suffer from an itchy and burning rash on the tip of their penis if they have had unprotected intercourse with an infected woman19. As such, a condom should be used during sexual intercourse if a woman has an active yeast infection.
While a yeast infection is NOT a sexually transmitted infection / disease they do share similar characteristics such as burning and genital discharge. If in doubt, an STD test can be ordered to rule out that possibility.
Can genital candidiasis be prevented?
In both sexes the following may help to reduce the risk of developing a yeast infection:
- Wearing underwear that is made of more breathable materials such as cotton to prevent moisture build-up that encourages candida growth
- Avoiding highly scented soaps and bath products
- Drying the genitals properly after washing
- Using a condom during sexual intercourse (although sexual transmission is very rare)
If a woman suffers from recurrent vaginal yeast infections (i.e. they occur more than three times a year), there is some evidence that suggests that the use of intravaginal (applied to the inside of the vagina) or oral probiotics may prevent the infection from recurring20.
Diagnosing genital candidiasis
With the symptoms of genital candidiasis being very similar to the symptoms of a number of different genital infections, the process of diagnosing it can often be difficult when done through a physical examination alone. Therefore, the diagnosis will normally entail the treating doctor obtaining a sample of any discharge present and examining this under a microscope (this is often done in a lab as the doctor will send the sample for testing).
This enables the doctor to find out if there is an abnormal amount of the fungus present as well as rule out any other causes of the infection.
Treatment and outcome of genital candidiasis
There are a number of different treatment options available in the form of antifungal creams or vaginal suppositories, available either over-the-counter or with a prescription.
Dosages range from a single, one-day dose to multiple doses over a week of treatment. If the infection is mild or moderate it can be treated through the use antifungal medication in a single dose. These types of medications have a high success rate, however, short-course treatment is not always effective in those who have more resistant or recurrent infections.
There are also a few OTC (over-the-counter) options available. Always ensure that you have an accurate diagnosis from a doctor before treating yourself for the infection. Overusing OTC drugs can result in the infection becoming resistant to treatment. OTC options include:
- Miconazole (Micatin, Monistat)
- Clotrimazole (Gyne-Lotrimin, Mycelex)
- Terconazole (Terzol)
References
18. Talaei Z, Sheikhbahaei S, Ostadi V et al. Recurrent Vulvovaginal Candidiasis: Could It Be Related to Cell-Mediated Immunity Defect in Response to Candida Antigen?. International Journal of Fertility and Sterility. 2017;11(3):134-141. doi:10.22074/ijfs.2017.4883
19. Vaginal yeast infections | Womenshealth.gov. womenshealth.gov. https://www.womenshealth.gov/a-z-topics/vaginal-yeast-infections. Accessed May 23, 2019.
20. Cribby S, Taylor M, Reid G. Vaginal Microbiota and the Use of Probiotics. Interdiscip Perspect Infect Dis. 2008;2008:1-9. doi:10.1155/2008/256490