- Candida
- Causes of candidiasis
- Signs and symptoms of candidiasis
- Oropharyngeal / oesophageal candidiasis (oral thrush)
- Genital Candidiasis / vulvovaginal candidiasis (VVC) / Candidal vulvovaginitis
- Cutaneous Candidiasis / Candida Skin Infection
- Invasive candidiasis
- What is Candida die-off?
- Candida Diet and Outlook for the infection
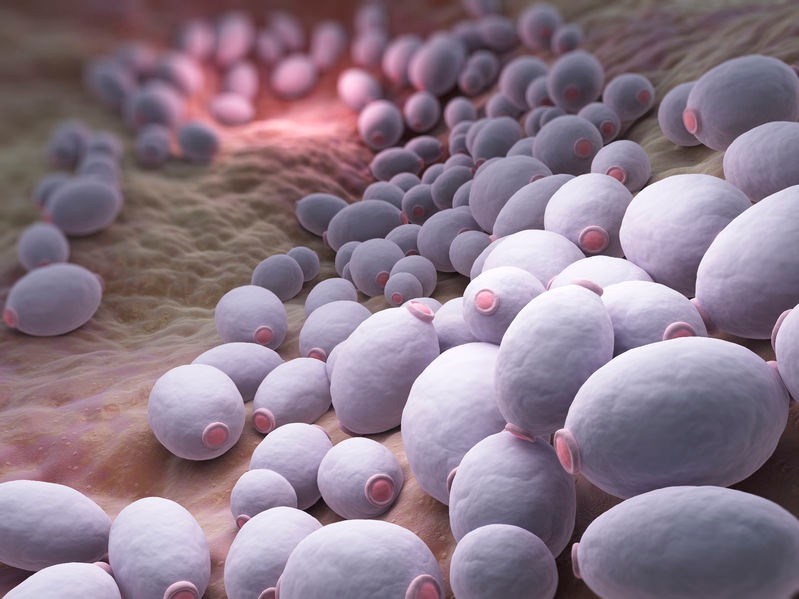
What is Candida?
A number of different fungi exist in our bodies at any given time. Candida is one of the better-known naturally occurring fungal residents. It is a type of yeast that typically exists in small amounts on the skin, in the mouth and gastrointestinal tract as well as in the vagina. In its natural state, when occurring at optimal levels, its presence does not cause any issues. Within the gut it actually aids in the absorption of nutrients and digestion.
If, however, changes in the balance of the body's natural environment occur for some reason (usually due to illness or the use of certain medications), this fungus can grow and multiply at a rapid pace, resulting in a fungal infection known as candidiasis1 (pronounced 'kan-di-dahy-uh-sis').
While there are over 200 different species within the Candida genus (family or group) only a few cause infections in humans2. Candida Albicans (C. Albicans) is most often associated with candida infections.
In recent years people's susceptibility to candidiasis has increased due to the overuse of antibiotics, the use of catheters, endoscopes and other invasive devices during surgical procedures, the increase in organ transplants as well as growth in the number of HIV/AIDS infections.
In cases where candidiasis develops as a result of surgery, the instruments used in these procedures may form the point of entry for Candida to access the blood stream (as it resides on the skin or the instrument becomes infected with it) and cause an infection in those suffering from immunosuppression (a compromised immune system). When this occurs, the infection is referred to as invasive candidiasis.
While most candida infections can be treated with over-the-counter (OTC) or prescription medications, in the case of more severe candidiasis, the diagnosis and treatment is far more complex and intricate, as are the severity of the symptoms experienced by the sufferer.
What are the different types of candidiasis?
The four main types of candidiasis3 are:
- Oropharyngeal / oesophageal candidiasis (i.e. yeast infection of the mouth, throat and oesophagus, commonly referred to as oral thrush)
- Genital / vulvovaginal candidiasis (commonly referred to as vaginal thrush)
- Cutaneous candidiasis (i.e. a yeast infection of the skin most commonly manifesting as irritation under women's breasts, in the armpits or groin areas of both genders and as diaper / nappy rash in infants)
- Invasive candidiasis (a serious infection affects various parts of the body including the blood, heart, eyes, brain and bones).
References
1. Vaginal Candidiasis | Fungal Diseases | CDC. Cdc.gov. https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html. Published 2019. Accessed May16, 2019.
2. Spampinato C, Leonardi D. Candida Infections, Causes, Targets, and Resistance Mechanisms: Traditional and Alternative Antifungal Agents. Biomed Res Int. 2013;2013:1-13.doi:10.1155/2013/204237
3. Candidiasis | Types of Diseases | Fungal Diseases | CDC. Cdc.gov. https://www.cdc.gov/fungal/diseases/candidiasis/index.html. Published 2019. Accessed May 16, 2019.
Other Articles of Interest

Diabetes (Diabetes Mellitus)
Diabetes (diabetes mellitus) is a long-term disease that requires daily management and care. The illness refers to a group of metabolic health conditions. Learn about the different types here...

HIV/AIDS
Since the early 1980s, HIV/AIDS has been widely publicised as a destructive virus without a cure. We take a look at what the condition is and how to treat it for the best quality life possible...

Nappy Rash
What is nappy (diaper) rash? Nappy rash is not a disease, but rather a condition where inflammation affects the surface of the skin. Here's all you need to know...
