How are cataracts treated?
Once testing and evaluations are complete, a doctor will make a diagnosis and assess whether vision impairments can be corrected or if other treatment measures may be required to provide ways for a person to make the most of what vision quality they have left. This can include:
- Ensuring that contact lenses or eye glasses are the most accurately effective prescription
- Suggesting a magnifying glass for reading purposes (especially fine print)
- Making use of brighter lamps and light bulbs in the home or working environment (a soft background light and an additional light illuminating a particular action directly, such as reading can help)
- Avoiding glare from screens (television or computer screens or mobile devices)
- Wearing good quality sunglasses (sometimes with an anti-glare coating) when outdoors and or / a wide-brimmed hat to assist with reducing glare
- Avoiding or limiting driving at night
- Rearranging the home in such a way that assists with preventing injury and makes living with low vision a little easier and more hazard-free
- Making use of low-vision aids such as video enlargement systems and computerised speech software
- Cutting down or quitting smoking to slow down the progression of cataracts
When should surgery be considered?
When cataracts are having a considerable impact on a person’s quality of life, it is most likely that a doctor will discuss surgical removal following a diagnosis. Currently, surgery is the only effective means to treat and remove a cataract from the eye/s.
Surgery is an elective procedure and can be scheduled according to a patient’s earliest convenience. Surgery is most often recommended by a doctor when cataracts have advanced to a stage that prevents a good quality of life in one’s day-to-day living. It is also the best option if a person wishes to be able to continue driving a car. Those who live in a retirement or assisted-living facility may prefer to avoid surgery and rather make use of vision aids (glasses etc.). The choice is a personal one and is most often, entirely up to the individual involved.
Surgery can be delayed in some instances, for several months or even years. Delaying surgery may not cause further long-term damage to the eye, result in the development of pain or make the procedure more difficult to perform later on. Progressive cataracts merely affect visual capability. A doctor may however make surgical recommendations as the preferred method of treatment, especially if a cataract coincides with another eye-related problem, such as macular degeneration, optic nerve damage, diabetic retinopathy or glaucoma (a group of eye conditions which lead to blindness). This is because the underlying condition can worsen the extent of cataracts and thus a person is better off with having them removed. In other instances, cataract removal may not improve visual capability at all. A doctor will discuss the best recommended course of action based on the individual and the extent of eye abnormalities experienced.
Surgery is generally considered safe (with few complications) and has a very high success rate (up to 90%) (1). In general, where the only issue is cataracts, a person has a very high chance of improved vision post-op. A person may still require reading glasses or prescription glasses for near vision, but overall vision can be considerably improved.
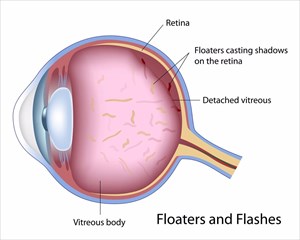
Surgery does carry some degree of risk for infection or bleeding (haemorrhage), as well as retinal detachment (signs of this are considered a medical emergency and include a sudden increase in flashes or ‘floaters’ – specks that appear to float in a person’s field of vision, causing permanent loss of vision), but this rarely occurs. To lower the risk of bleeding a doctor may request that use of certain medications (where applicable) be temporarily discontinued shortly before surgery.
It is advisable to talk to the diagnosing doctor about whether surgery is the best possible option. For progressive cataracts, surgery is the best option when interference is considerable and the ability to perform daily tasks or activities is greatly impacted. No instance of cataracts need reach a stage of total blindness, but for many individuals there is no immediate need to dash into surgery.
All surgical benefits and risks should be discussed and carefully considered before a decision is made. If surgery is not elected in the short-term, a doctor may recommend periodic follow-ups to monitor possible progression of cataracts.
How will surgery for cataracts be performed?
Prior to surgery (about a week or two beforehand), the attending doctor will request a consultation to measure the curve of the cornea, and the overall shape and size of the eye (this is applicable for implant purposes). Prior to the procedure, the doctor will request that no food or liquid be taken for a period of time (allowing for the stomach to be empty at the time of surgery which leads to fewer complications while sedated).
Most individuals are booked into hospital on an outpatient basis and return home on the same day. Ahead of surgery, the doctor will place dilating eyedrops in the eye in order to enlarge (dilate) the pupil, as well as cleanse the eye area.
A local anaesthetic is usually given (intravenously) for light sedation ahead of surgery (others may opt for general anaesthetic and be completely unconscious for the procedure). A person will be made comfortable for the duration of the procedure and generally not feel a thing (the nerves around the eye area will be completely numbed). The surgery is normally performed in just under half an hour or up to 1 hour.
Surgical techniques which may be used include:
- Phacoemulsification (small incision surgery): Small incisions are made and ultrasound waves are then used to break apart the cataract for easier removal. A doctor may also make use of a laser to perform the surgery and remove the cataract.
- Standard extracapsular cataract extraction (ECCE): A long incision is made in the cornea or front portion of the lens capsule and the opaque portion of the lens is carefully removed (as one piece).
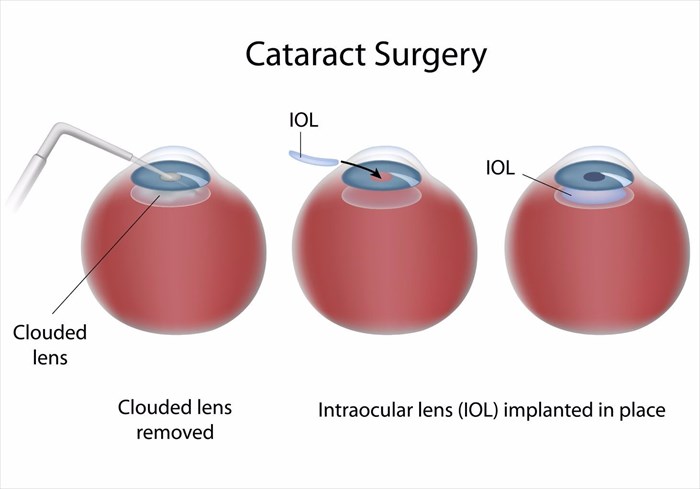
An artificial intraocular lens (IOL implant) is placed where the natural lens was to aid in improving vision. This is done at the same time as the cataract removal procedure. Removing the cataract essentially also means removing a portion of the natural lens (capsule) of the eye. A portion of the lens capsule is left so as to support the implanted IOL lens. The implant is intended to remain permanently, and as discussed, measurements for the size, shape and power of the IOL implant will have been determined ahead of surgery. In instances where an implant cannot be used (such as in the case of multiple eye problems), a doctor may prescribe new glasses or contact lenses as a way to help correct vision problems.
The option for using an IOL implant will likely be discussed prior to surgery. If an individual elects not to have the implant, or a doctor does not recommend one (often due to the nature of other medically related eye problems or diseases), prescription glasses or contact lenses will be discussed. A doctor will ensure that if contact lenses are preferred, an individual is well-informed about how to use them on a daily basis (educating the patient on how to insert, remove and clean them). Contact lenses are most often not preferred for young children or older adults who may not be comfortable using them.
Once surgery has been completed, a doctor will place a patch over the eye, and before being discharged, a patient will be carefully monitored for a short time to look for any signs of complications, such as bleeding. A patient is advised to arrange for safe transport home following surgery, and not to attempt to drive themselves.
What happens after surgery
Following surgery, vision will temporarily be a little blurry due to the effect of the dilating eyedrops used to enlarge the pupil and until the swelling of the eye reduces. Healing generally takes place for up to 8 weeks following cataract removal. A person can expect a little discomfort for a few days, and sometimes a little itching and fluid discharge from the eye/s. During the first few days, the eye/s will also be a little light sensitive and tender, so direct touching should be limited or avoided. Moderate discomfort should ease within a day or two.
Medications may be prescribed to reduce the risk of potential infection. A doctor will also recommend keeping the eye covered with a patch and / or glasses for a period of time while healing to protect the it, especially while sensitive, and to reduce the risk of injury (accidental bumping or rubbing).
Normally a doctor will recommend prescription eyedrops following surgery and provide care details for protecting the eye from any damage, including infection. Eyedrops may be used for a few weeks post-op to help promote healing.
A doctor will also advise that an individual ‘takes things easy’ in the days post-op and does not engage in activities requiring the lifting of heavy objects. Light walking and household chores should be fine and not cause any problems while healing.
Once healed it may be determined that prescription eye glasses or contact lenses will need to be acquired due to new vision changes.
If both eyes are affected by cataracts, a doctor will have only performed a removal on one eye, and will schedule surgery for the other at a later stage, once the eye operated on has sufficiently begun healing. It’s important for the eye which was operated on to heal (before the second surgery procedure is performed) so that a doctor can determine to what degree a person’s eyesight has improved post-op.
During healing, routine check-ups may be recommended to assess progress and evaluate any potential improvements in vision. A doctor will also stress the importance of taking care of the eyes and recommend protective measures, such as good quality sunglasses which offer glare protection, brimmed hats, as well as good nutrition (especially green leafy vegetables, foods rich in antioxidants and fruit) which contribute to lowering the risk of age-related cataracts.
Older individuals may also be requested to keep consistent and regular eye examinations (at least once every year or two) to monitor overall eye health and ensure any signs of macular degeneration or other vision diseases and disorders are picked up early. Early detection can prevent permanent loss of vision.
Can vision return to normal following surgery?
A full recovery does take time, but a person can safely return to normal activity reasonably quickly and experience much improved vision quality. The healing eye gradually adjusts and almost ‘re-learns’ how to focus again, along with the other eye. It is advisable to ensure that a doctor has given approval to engage in certain activities, such as driving before resuming normal lifestyle.
If an IOL implant was used, colours may initially appear to be quite bright and vivid (in comparison with the clouded lens and cataract which was removed). The yellowish / brownish tint once experienced should no longer exist. It may take some time for a person to get used to the improved colour and overall vision clarity.
What are the most common potential complications of cataract surgery?
An ‘aftercataract’ is not considered too serious a complication and can be relatively simple to treat – usually with a laser surgery procedure (known as a YAG laser posterior capsulotomy). A laser is used to make an opening in the affected lens capsule, which allows more light to enter the lens. In this way, vision clarity can be restored. The procedure is quick to perform (and is often performed in a matter of minutes), painless and takes place in the specialist’s office. It is rare for complications, such as increased eye pressure, to occur as a result of the procedure. Eyedrops will be given before and after the procedure to assist with maintaining normal eye pressure.
Other complications of cataract surgery (although rare) include:
- Bleeding (haemorrhage) or other type of eye discharge
- Infection
- Inflammation (swelling, redness and pain usually associated with a very dense cataract which interfered with fluid drainage or protein leakage from within the eye)
- Increased or decreased eye pressure
- Displacement of the IOL implant
- Loss of a portion of the broken-up cataract in the eye
- Double vision
- Glaucoma
- Retinal detachment (floaters, changes in field of vision and flashes of light)
- Blindness (loss of vision)
If any complications occur, the treating doctor or specialist must be consulted as soon as possible to effectively evaluate and provide necessary medical assistance.
Reference:
1. National Eye Institute (NEI). September 2015. Facts about Cataract: https://nei.nih.gov/health/cataract/cataract_facts [Accessed 30.08.2017]