Signs and symptoms of Ebola virus infection
Incubation period
During primary transmission cases, the incubation period for the Ebola virus (i.e. the time period between the date of exposure to the virus and when the signs and symptoms of illness become most apparent) is most commonly between 3 and 8 days. This may be slightly longer in instances of secondary transmission (i.e. contact with a person or primate that is infected). Incubation periods, however, may be slightly varied with some infected individuals only experiencing notable symptoms between 19 and 21 days after exposure.
Early signs and symptoms
Once indications of illness develop, the onset of Ebola virus symptoms is typically abrupt and acute (i.e. requires urgent care). Once symptoms develop, the virus is likely to have begun multiplying in the bloodstream and other bodily fluids, and thus a person is considered infectious to others.
The onset of symptom development may vary, occurring in as little as a few days following exposure, to between 6 and 12 days (sometimes longer). Some outbreak averages have been estimated at between 8 and 10 days. In general, symptoms are likely to develop within 21 days following exposure to the virus.
Any person who experiences symptoms associated with the Ebola virus, who may have been exposed to a living or deceased individual with the condition (whether confirmed or suspected) or who has recently travelled to an area with a history of outbreaks and begins to feel unwell, must consult a medical professional immediately for evaluation.
The initial (acute) signs and symptoms which will develop when a person is infected with Ebola virus include:
- Fever (low-grade) – with or without body chills
- Body weakness (asthenia), general malaise and fatigue
- Diarrhoea (watery stools – sometimes up to 10 litres a day in severe instances in adults) (4)
- Myalgia (muscle discomfort or pain)
- Arthralgia (joint pain)
- Headache (this may be severe)
- Nausea and vomiting
- Abdominal discomfort or pain
- Pain when swallowing (odynophagia) or swallowing difficulties (dysphagia)
- Loss of appetite
- Conjunctival injection / conjunctivitis (red eye/s), sometimes accompanied by blurred vision, pain, blindness and photophobia (light sensitivity)
If not promptly treated, gastrointestinal symptoms (such as vomiting and diarrhoea) can lead to severe fluid loss which can quickly result in complications including dehydration, low blood pressure (hypotension) and a state of shock.
Some individuals (not all infected people) may also experience the following:
- A high-grade fever
- A maculopapular rash (small confluent bumps that are not itchy and accompanied by redness) – The rash typically develops on the face, neck, trunk and arms. Bumps can develop flakes or scales which are shed from the body. The rash is easier to identify in fairer complexion individuals. If a rash develops, it typically affects a person within 5 to 7 days following Ebola virus exposure.
- Bradycardia (an abnormal slowing of heart function) – often accompanied by pulse-temperature dissociation
- Pericarditis (a swelling of the membrane surrounding the heart muscle)
Progressive signs and symptoms
A person’s condition can progressively worsen with more severe signs and symptoms developing. Some of these can include:
- A masked facial expression (also referred to as expressionless facies)
- Unexplained bleeding (bruising (ecchymoses) as well as internal and external haemorrhage – bleeding can occur at the site where intravenous / IV lines are administered or through mucous membranes, stool / faeces, and broken capillary blood vessels in the skin). Haemorrhage is most typical of a person whose condition has reached a terminal stage or in pregnant women.
- Inflammation of the heart muscle (Myocarditis)
- ‘Wet lung’ / an accumulation of fluid in the lungs (pulmonary oedema)
- Rapid breathing (tachypnoea) and shortness of breath (hypoxia or hypoventilation may occur following respiratory muscle fatigue)
- Low blood pressure (hypotension)
- Kidney dysfunction – including a failure to produce urine (anuria)
- Meningoencephalitis (inflammation of the brain) – typical signs include altered levels of consciousness, a stiff neck, gait instability (i.e. changes in the way one walks), overactive / over-responsive reflexes (hyperreflexia), muscle dysfunction (myopathy) and seizures. This can develop within 8 to 10 days following Ebola virus exposure.
- Coma
Risk factors for Ebola virus infection
1. Location
Transmitted infections are typically localised to the regions in which Ebola virus outbreaks occur and the risk of infection is typically highest for those within the area where an outbreak has taken place.
The criteria for high-risk individuals includes:
- Anyone with a travel history to sub-Saharan Africa (especially countries such as DRC, Sudan, Gabon, Côte d'Ivoire, Uganda, Guinea, Liberia and Sierra Leone)
- Healthcare workers who have been exposed to infected individuals
- Individuals who have worked with or handled primates
A few reported cases of Ebola have occurred in non-outbreak prone countries. In these instances, international healthcare personnel have been transported out of an outbreak area to their home countries for treatment and infected others. To date, these instances have been rare and not caused enough risk for widespread panic (i.e. infections as a result were quickly identified and contained).
2. Gender and age
It has been noted in past Ebola outbreaks that fewer children than adults have contracted the Ebola virus. Mortality rates among children have been somewhat lower as a result. (5) It is believed that children are typically exposed to infected individuals less frequently than adults, but this does not mean that they are not still at risk.
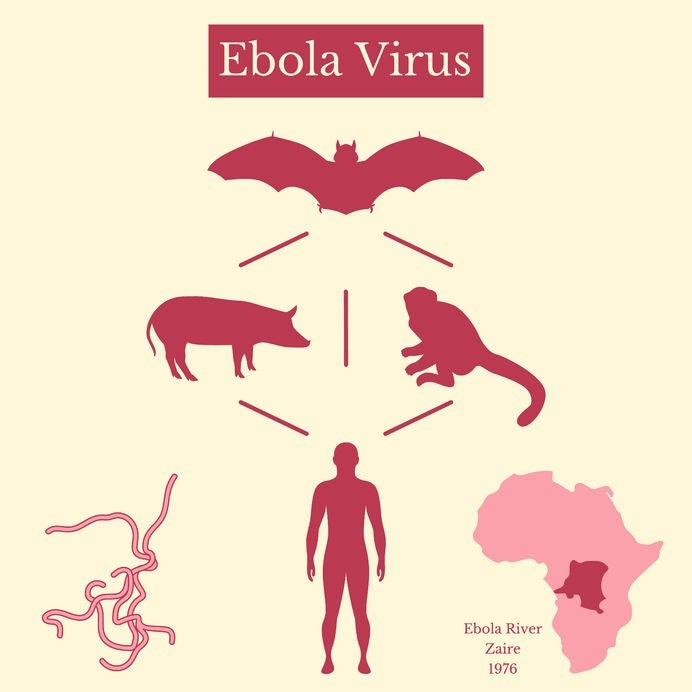
Adult males appear to be at higher risk of primary transmission infection than females, especially if they frequent forested and savanna areas close to their villages and towns. Many who frequent these areas source animal (specifically primate) carcasses or hunt potentially infected species which are then used as food (bushmeat). Contact with infected bats during hunting or otherwise, can also occur. Adult females appear to be more at risk when caring for family members who become infected.
Females are also regularly involved in preparing the bodies of deceased loved ones for burial rituals. If these individuals have died as a result of the Ebola virus, infection may be acquired through direct handling or contact with an infected person. Females may also be at higher risk if engaging in sexual activity with men who have recently contracted Ebola or survived an infection after receiving effective treatment.
3. Healthcare personnel
Healthcare workers of either gender become high-risk individuals when providing medically supportive care to patients infected with the Ebola virus. Within a medical care facility, all who are present are in close contact with one another. Infections may be acquired through the direct handling of infected individuals or through contact with contaminated objects and surfaces. Thus, healthcare workers are considered to be at an equal risk of infection as those who are already under treatment.
Strict safety measures for the handling of patients including the wearing of protective clothing and equipment, as well as the safe disposal or disinfection of tools and medical supplies can help to significantly reduce the risk of transmission in healthcare workers.
Overview history of Ebola outbreaks – human-to-human transmissions (6)
| Year of Outbreak / Occurrence | Outbreak / Occurrence Locations | Ebola Virus Species | Cases Reported & Fatality Rate *includes confirmed, probable and suspected cases |
| 2018 | DRC | Zaire ebolavirus | Active (reported cases and fatality rates are ongoing) As at 21 May 2018:
|
| 2017 (May – July) | DRC | Zaire ebolavirus |
|
| 2015 | Italy | Zaire ebolavirus |
|
| 2014 |
|
Zaire ebolavirus | Reported cases and fatality percentage:
|
| 2014 - 2016 |
|
Zaire ebolavirus | Reported cases and fatality percentage:
|
| 2012 |
|
|
Reported cases and fatality percentage:
|
| 2011 | Uganda | Sudan ebolavirus |
|
| 2008 | DRC | Zaire ebolavirus |
|
| 2007 |
|
|
Reported cases and fatality percentage:
|
| 2005 | Congo | Zaire ebolavirus |
|
| 2004 | Sudan | Sudan ebolavirus |
|
| 2003 | Congo / DRC
|
Zaire ebolavirus | Reported cases and fatality percentage:
|
| 2001 - 2002 |
|
Zaire ebolavirus | Reported cases and fatality percentage:
|
| 2000 | Uganda | Sudan ebolavirus |
|
| 1996 |
|
Zaire ebolavirus | Reported cases and fatality percentage:
|
| 1995 | DRC | Zaire ebolavirus |
|
| 1994 |
|
|
Reported cases and fatality percentage:
|
| 1979 | Sudan | Sudan ebolavirus |
|
| 1977 | DRC | Zaire ebolavirus |
|
| 1976 |
|
|
Reported cases and fatality percentage:
|
Overview history of Reston ebolavirus outbreaks
| Year of Outbreak | Outbreak Locations | Cases Reported (No Fatalities) *includes confirmed, probable, suspected and unproven cases |
| 2008 | Philippines (associated with pig farming) | Cases reported: 6 |
| 1996 | Philippines | No reported cases were proven |
| 1992 | Italy | No reported cases were proven |
| 1990 | USA Virginia and Texas Alice (Texas) |
Cases reported: 4 * No reported cases were proven |
| 1989 - 1990 | Philippines | Case reported: 3 |
| 1989 | USA (Virginia, Texas, Pennsylvania) | No reported cases were proven |
References:
4. ATS Journals. November 2014. Clinical Presentation and Management of Severe Ebola Virus Disease: https://www.atsjournals.org/doi/full/10.1513/AnnalsATS.201410-481PS [Accessed 23.05.2018]
5. U.S. National Library of Medicine - National Institutes of Health. March 2015. Ebola in children: epidemiology, clinical features, diagnosis and outcomes: https://www.ncbi.nlm.nih.gov/pubmed/25522340 [Accessed 23.05.2018]
6. World Health Organization. February 2018. Ebola Virus Disease - Key Facts: http://www.who.int/en/news-room/fact-sheets/detail/ebola-virus-disease [Accessed 23.05.2018]