Ebola virus prevention
Outside of the African continent, the prevalence of Ebola (or EVD) is considered extremely rare. Within sub-Saharan Africa, where the majority of outbreaks have taken place, the disease is more frequently encountered and widespread.
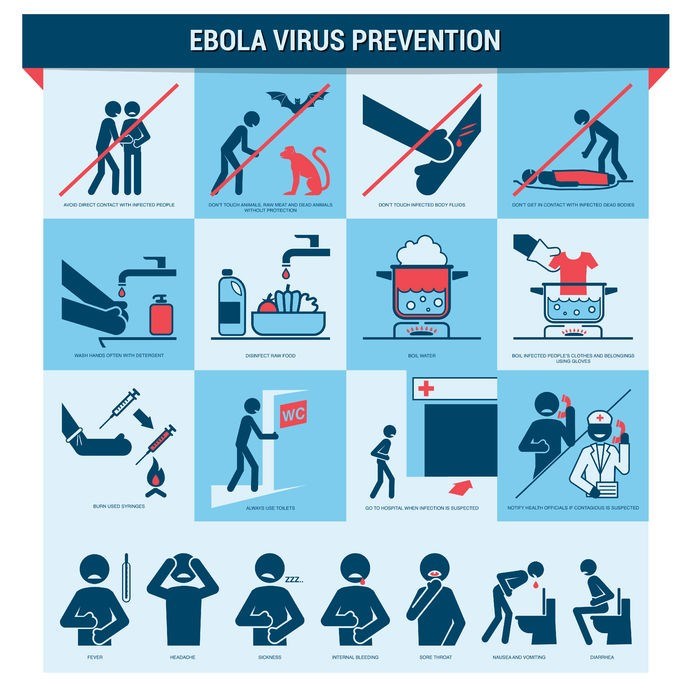
Prevention of Ebola mostly relates to individuals living in or travelling to regions where the Ebola virus has historically occurred. There are several factors to take into consideration when it comes to its prevention…
General preventative measures
1. Hygiene and handwashing
Direct contact with bodily fluids can lead to the virus entering the body through broken skin or the mucous membranes (mostly those of the eyes, mouth or nose). Hands which come into contact with the infected blood or bodily fluids of a symptomatic individual can often transmit the virus via the mucous membranes just by touching the facial area. Mindful hand hygiene is thus one way the risk of transmission can be lowered, reducing the spread of further infection.
Hand hygiene considerations for prevention can include:
- Soap and water: Antimicrobial soaps can be used, although plain soap and warm water is also sufficient for removing visible dirt or soiling from blood or other bodily fluids. Hands must be washed thoroughly and dried with clean cloths or towels.
- Alcohol-based hand sanitisers: Products that contain between 60% and 95% ethanol isopropanol (alcohols) can be effective. These are best used when the hands are not visibly soiled (i.e. with blood or other bodily fluids) but have been potentially exposed to these.
2. Avoidance considerations and reducing Ebola transmission risk
If and when a person is in a region or country known to experience Ebola outbreaks, the following considerations are highly advisable:
- Reducing the risk of human-to-human transmission: Avoid direct contact with blood and bodily fluids or substances including saliva, sweat, urine, faeces, vomit, breast milk, vaginal fluids or semen. Avoid contact with items and objects that may have been exposed to an infected individual’s blood or other bodily fluids and substances, including bed linens, clothing and even medical equipment (like needles or syringes). Avoid direct contact with the physical body of an individual who has died from an Ebola infection. This includes contact associated with burial rituals and funeral processes.
- Reducing the risk of animal / wildlife-to-human transmission: Avoid direct contact with non-human primates or bats, as well as the blood or other fluids of raw meat used from either of these species or any other from an unidentified / unknown source. If handling animals for food consumption purposes, the wearing of gloves and protective clothing is strongly advised. Animal products should also be thoroughly cooked before being consumed.
Anyone who has travelled to an area with a known history of outbreaks should remain alert with regards to their overall health condition for at least 21 days after returning home. If any signs and symptoms of ill health develop within that time period, a medical consultation must be arranged immediately.
3. Reducing the risk of sexual transmission
The risk of sexual transmission of the Ebola virus is not entirely well understood but it is believed to be a significant possibility. Thus, it is advised that sexual activity (without sufficient protection) with an individual who has recovered from the Ebola virus be avoided.
The greater risk appears to be for the partners of men who have had the Ebola virus and made a recovery. Just how much of the virus remains in semen and over what period of time during recovery is yet to be determined. It has been documented as a possibility for transmission to occur up to 9 months after falling ill with Ebola virus. (9) Nevertheless, transmission through sexual activity is not considered a primary risk. Instead it has been documented as a rare instance. However, evidence-based possibility is something that has encouraged further research in order to conclusively determine related risk factors, including whether or not women in recovery may pose a risk to their partners too (through contact with vaginal fluids).
Once a patient is ready for clinical discharge and can continue recovering in a home setting, healthcare workers are likely to provide some counselling to a survivor and their sexual partner. The counselling will detail the risk involved when it comes to sexual transmission. Condoms may also be provided in order to encourage enhanced protection for both men and women.
Survivors and their sexual partners can then choose to either completely abstain from any form of sexual activity or observe safe sex practices with the use of condoms until such time as a previously infected male’s semen has tested negative for the virus at least twice.
For male survivors, semen testing (RT-PCR) is offered within 3 months (from the onset of disease symptoms). Should this test return with positive results, a medical professional will recommend follow up tests at least once every month thereafter until such time as results return as negative. At least 2 consecutive negative results (conducted at least 1 week apart) are considered clear of the virus. Normal sexual activity is then considered safe and virus free.
Until such results are obtained, general hygiene practice is just as important as practicing safe sex. Survivors and their partners must ensure proper hygiene and handwashing immediately after any physical contact with semen is made. Used condoms must be carefully disposed to reduce the risk of contact with infected semen.
Ebola vaccines
Currently there is no vaccine for the Ebola virus that has officially been licensed for use anywhere in the world. Numerous candidates are, however, undergoing extensive research processes. The different candidates are at different development stages too.
Vaccine candidates which have shown the most promise at this stage include: (10)
- NIAID/GSK investigational Ebola vaccine (or cAd3-EBOZ): This vaccine was developed by the U.S. Army Medical Research Institute of Infectious Diseases and Okairos (taken over by GlaxoSmithKline / GSK). The vaccine is based on a type of adenovirus in chimpanzees (cAd3 / chimp adenovirus type 3) which functions as a carrier for the delivery of Ebola genetic material (i.e. it does not contain any Ebola virus material). The adenovirus is a viral carrier that doesn’t replicate - meaning that it is capable of delivering the gene of the Ebola virus, while hindering any further replication, and inducing an immune reaction in the body instead. The vaccine underwent clinical trials (phase 1) in the USA and UK during 2014, and phase 2 and 3 during 2015 (February). Collective findings showed that the vaccine could be tolerated well and was successful at inducing an immune reaction, which could be significantly helpful in protecting against Ebola virus infection.
- rVSV-ZEBOV Ebola vaccine (recombinant vesicular stomatitis virus–Zaire Ebola virus): Canada’s Public Health Agency developed the vaccine and has been licensed to Merck & Co. The National Institute of Allergy and Infectious Diseases has been involved in testing procedures in the quest for regulatory use approval. The vaccine makes use of the vesicular stomatitis virus (which predominantly affects cattle) to function as the carrier of Ebola virus genes. The vaccine also does not contain any Ebola virus material. As with cAd3-EBOZ, this vaccine is designed to promote antibody (immune) responses so as to fend off an Ebola virus infection. The vaccine has undergone phase 1 and phase 2 clinical trial testing. In February 2016, this vaccine too indicated that it could be tolerated well and achieve the induced immune responses required for it to work effectively.
These two potential Ebola vaccines have shown significant promise for possible approved use. Both are capable of inducing immune responses in the body within 1 month. The induced immune response can also last for up to 1 year (offering a vaccinated individual sustained immunity). (11)
Neither or the two vaccine candidates caused any major use health complications during trials. Side-effects experienced by those participating in research studies have been recorded as minor and transient (temporary).
Side-effects may include:
- Swelling at the vaccination site
- A low-grade fever
- Fatigue
- Headache
- Muscle discomfort or pain.

In 2016, an outbreak of Ebola occurred in Guinea and the rVSV-ZEBOV vaccine was given authorisation for use outside of research settings. A total of 1 510 individuals were vaccinated, including minors (between the ages of 6 and 17) and front-line workers. No severe side-effects were noted (minor side-effects were experienced for a short period). None of the vaccinated individuals contracted the Ebola virus either. A ring vaccination strategy (immunising large groupings of individuals in a short period of time) was also shown to be an effective means of implementation. (12)
Research for these vaccines and others is also ongoing, including one which may be used in primates at risk of infection with the Ebola virus.
References:
9. U.S. National Library of Medicine - National Institutes of Health. May 2016. Potential Impact of Sexual Transmission on Ebola Virus Epidemiology: Sierra Leone as a Case Study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4852896/ [Accessed 23.05.2018]
10. National Institutes of Allergy and Infectious Diseases. February 2016. Ebola Vaccines: https://www.niaid.nih.gov/diseases-conditions/ebola-vaccines [Accessed 23.05.2018]
11. U.S. Department of Health and Human Services - National Institutes of Health. October 2017. Progress on two Ebola vaccines: https://www.nih.gov/news-events/nih-research-matters/progress-two-ebola-vaccines [Accessed 23.05.2018]
12. U.S. National Library of Medicine - National Institutes of Health. Decmber 2017. Ring vaccination with rVSV-ZEBOV under expanded access in response to an outbreak of Ebola virus disease in Guinea, 2016: an operational and vaccine safety report: hhttps://www.ncbi.nlm.nih.gov/pubmed/29033032 [Accessed 23.05.2018]