What is meningitis?
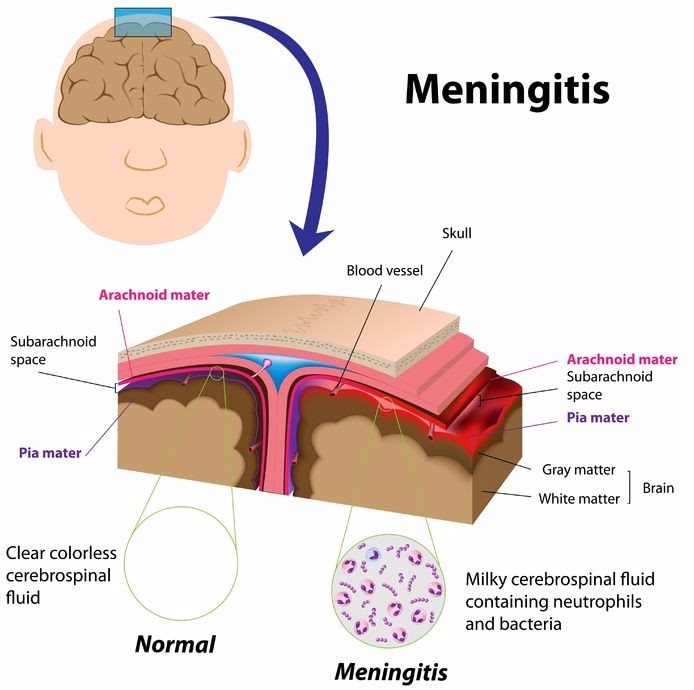
An inflammation or swelling on the delicate meninges (three protective membranes surrounding the brain and spinal cord), meningitis is typically caused by a viral, bacterial or fungal infection of the surrounding cerebrospinal fluid. Meningitis can also occur due to injury, fungi, chemical irritation, cancer or drugs and medication allergies.
Inflammation of the meninges results in typical symptoms of headache, fever and a stiff neck. Treatment for meningitis is dependent on the cause and will differ accordingly.
Meningitis can be a life-threatening condition, requiring urgent antibiotic treatment to prevent potentially severe complications.
If you suspect meningitis, it is best to see a medical professional as quickly as possible. The sooner this condition is treated, the less the risk for further complications. An infection can escalate quickly if not sufficiently identified and adequately treated.
Other Articles of Interest

MRI (Magnetic Resonance Imaging)
What is an MRI? How does it work? What does it test? What can you expect to experience during the procedure? Here's everything you need to know...

HIV/AIDS
Since the early 1980s, HIV/AIDS has been widely publicised as a destructive virus without a cure. We define what the condition is and how to go about getting the best treatment possible...

Food poisoning (foodborne illness)
Foodborne illness is most often referred to as food poisoning. What exactly is food poisoning? What causes it and how is it best treated? Learn more here...