- Blood clot
- Types and causes of blood clots
- What risk factors contribute to blood clots?
- What are the signs and symptoms of blood clots?
- What kinds of blood clot complications can occur?
- How are blood clots diagnosed?
- What treatment procedures are involved in dealing with blood clots?
- Are there ways to prevent blood clots and what are the associated complications?
- Blood clot FAQs
Different types of blood clots
Types of clots based on movement2. These are categorised as follows:
- Thrombosis: This refers to a clot that is stationary and does not travel through the bloodstream.
- Embolus: This refers to a clot (or a portion which has broken free) that moves and travels through the blood vessels to another part of the body.
Types of clots based on location
- Arterial: A thrombus (blood clot) forms in the arteries (i.e. the blood vessels which carry oxygenated blood away from the heart and circulate the body’s tissues). Clots effectively prevent life-giving blood and oxygen from reaching these tissues and thus result in damage. Arterial clots can affect the feet, legs, heart, kidneys, intestines and even the eyes (although this is rare).
- Venous: These clots form in the veins and typically develop gradually. This is often why a thrombus may go unnoticed until complications occur. Three types of thrombosis generally occur in the veins – superficial venous thrombosis (form in the small veins close to the skin’s surface), deep vein thrombosis (or venous thrombosis whereby clots form in the deeper, major veins of the body) and pulmonary embolism (a medical emergency whereby a DVT clot has travelled to the lungs). Venous clots typically affect the thighs, lower legs, pelvis, arms, intestines, liver, kidneys and brain.
What causes blood clots?
Abnormal blood clots can form for a variety of different reasons. Some of these include:
- Damage to the veins and arteries as a result of:
- Wounds or cuts (lacerations or tears).
- Slowing down of blood flow (stagnation).
- Genetic and/or medical conditions which cause hypercoagulation (abnormal clotting resulting in narrowing of the arteries or the excess production of platelets and red blood cells).
- Genetic and/or medical conditions which prevent the normal breakdown of clots when they are no longer needed (causing damage to the blood vessels and heart).
- Immobilisation of the body which causes a lack of muscle contraction (stimulating blood flow back to the heart), especially in the legs (venous thrombosis).
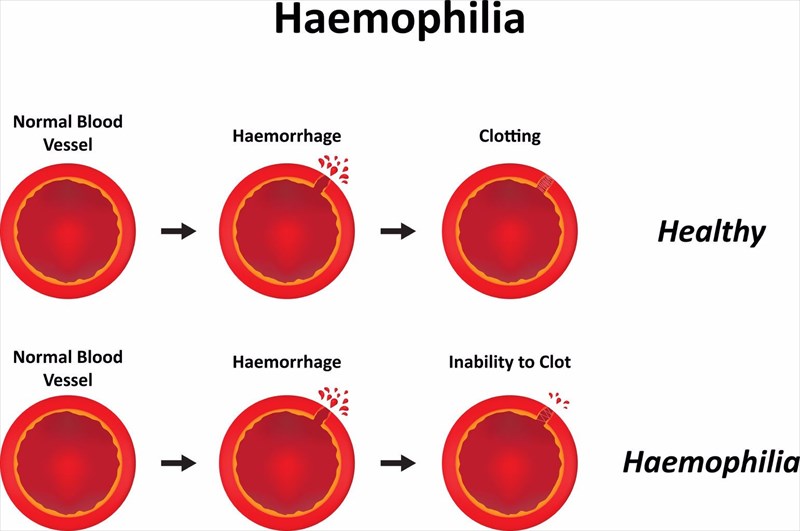
A thrombus / thrombi affecting the arteries increases the risk of serious complications such as stroke, heart attack or peripheral artery disease. Medical and/or genetic conditions associated with the formation of potentially harmful blood clots include arterial wall thickening or stiffness (or arteriosclerosis), atherosclerotic disease (deposition of atheroma/plaque), deep vein thrombosis, Factor V Leiden, peripheral artery disease, obesity, diabetes (increased plaque build-up), vasculitis (swollen blood vessels) hiatal hernia, haemophilia (a genetic condition), von Willebrand factor deficiency and polycythemia vera. Some medications containing oestrogen can also contribute to the formation of blood clots3, such as oral contraceptive pills (birth control pills) and hormone replacement therapy (HRT).
- Blood clots which occur as a result of heart conditions: The heart’s upper chamber (atrium) does not naturally beat in an organised manner and typically jiggles a bit in the case of atrial fibrillation (a condition characterised by a rapid or irregular heartbeat). In this instance, blood is affected and can become stagnant along the wall linings of the upper chamber of the heart. Over time, small clots can form in the ventricles, injuring the heart muscle (this can also happen following a heart attack) and disabling normal contraction function. The result is that blood begins to pool in the heart atria and ventricles, forming clots. These clots can be dislodged and travel to the brain resulting in a stroke. Other associated heart conditions which can result in blood clots include heart arrhythmias and heart failure (sluggish blood flow). Waxy cholesterol build-up (or plaque) in the arteries can also suddenly rupture (plaque rupture) or break open and result in a clotting process which can lead to heart attack.
- Blood clots which cause other medical conditions or problems: Normal clotting processes can cause an imbalance in the system that, based on location in the body, can lead to other health problems. For instance, if blood occurs in the urine due to trauma or an infection, clots can form over the urethra and prevent the bladder from being able to empty as it normally would. This can cause urinary retention. Clots can also develop in a woman’s uterus and result in symptoms of pain as these are passed through the cervix. This can then lead to abnormal vaginal bleeding during menstruation (menorrhagia) or cause great pain and discomfort (dysmenorrhea) during normal menstruation (where blood pools in the vagina and forms clots before it is expelled from the body). Rectal bleeding problems can result in a clot forming and mixing with bloodied stool (faeces).
References:
2. MedlinePlus. August 2018. Blood Clots: https://medlineplus.gov/ency/article/001124.htm [Accessed 28.08.2018]
3. MedlinePlus. July 2018. Estrogen: https://medlineplus.gov/druginfo/meds/a682922.html [Accessed 28.08.2018]
