- Crohn’s Disease
- What is the difference between Crohn’s disease and ulcerative colitis?
- What are the symptoms of Crohn’s disease?
- What are the causes of Crohn’s disease?
- What are the risk factors and complications of Crohn’s disease?
- How does Crohn's disease affect the intestines?
- What are the types of Crohn’s disease?
- How is Crohn’s disease diagnosed?
- How is Crohn’s disease treated?
- What are the lifestyle changes that can be made and the outlook for Crohn's disease?
What is Crohn’s disease?
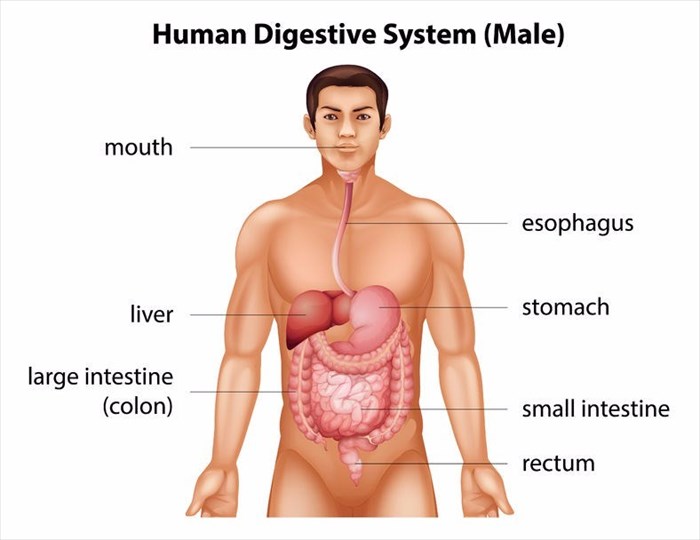
Crohn’s disease, which is also known as Crohn disease, is an inflammatory bowel (IBD) disease. It is chronic and causes breaks in the intestinal lining known as ulcerations. The small and large intestines are predominately affected, but the entire digestive system (gastrointestinal tract (GI)) from the mouth to the anus can also be impacted.
Crohn’s disease is named after the physician, Dr Burrill Bernard Crohn, who initially described the condition in 1932. It is also known as colitis, terminal ileitis, regional enteritis, ileitis or granulomatous enteritis.
Crohn’s disease is closely related to a different inflammatory condition involving only the colon and not the entire digestive tract, this condition is known as ulcerative colitis. These conditions are known as inflammatory bowel diseases, both of which have no cure. A number of people tend to confuse the two conditions although they are not the same thing. Both of the diseases will, however, fluctuate between remission (inactivity) and relapse (activity).
Crohn’s disease results in the digestive tract becoming inflamed, this typically leads to fatigue, severe diarrhoea, malnutrition and weight loss. The inflammation that is caused by the disease will spread into the layers of tissue that are affected and inflamed. This is often extremely painful and can be debilitating for the sufferer. Crohn’s disease can be life-threatening.
As stated, there is no cure for Crohn’s disease, however, there are a number of therapies that are able to significantly reduce its symptoms and in some cases, result in long-term remission. A number of patients who suffer from the condition are able to live healthy and normal lives.
More research into Crohn’s disease is needed as researchers are still unsure as to how the disease begins, who is more at risk of developing it and what the best method of treatment is. There have, however, been some major breakthroughs in the treatment of Crohn’s recently thanks to advances in technology.
Other Articles of Interest

Fever (Temperatures)
Often a sign that something is wrong in the body, a fever is a typical symptom of a variety of different illnesses. What happens when body temperature increases? When should you worry?

Diarrhoea
Suffering from a runny tummy? Having diarrhoea can often be an embarrassing and even painful experience. Find out all you need to know about dealing with and combating this condition.

Anaemia
Did you know that there are over 400 variations of anaemia? We define the condition, it's causes, symptoms and how to go about effectively treating it.