
- Thyroid Disorders
- Common types and underlying causes of thyroid disorders
- Signs and symptoms of thyroid dysfunction
- What risk factors are associated with thyroid disorder?
- Diagnosing thyroid disorders
- Treatment for thyroid disorders
- Common complications of thyroid disorders
- Outlook for thyroid disorders
1. Hyperthyroidism treatment
The treatment plan that a doctor will select is dependent on several factors:
- Age
- Overall physical condition
- Underlying cause of the overactive thyroid
- Severity of the condition
Treatment may involve blocking the production of excess hormones or destroying the gland altogether. Treatment options involve the following:
- Radioactive iodine: Taken orally, this treatment method has proved reasonable safe and effective for more than 60 years. The radioactive iodine is easily absorbed in the thyroid gland and has the effect of easing symptoms by shrinking enlarged glands. Effects are typically seen within 3 to 6 months of starting treatment. Treatment can, however, slow down hormone production activity, sometimes to the point of becoming underactive. In this instance, daily medication to replace T4 may be necessary. Side-effects of radioactive iodine can include dry mouth and eyes, fatigue, an altered sense of smell or taste and nausea. The drug typically exits the body through the urine.
- Anti-thyroid medications: Symptoms can be alleviated with medications that prevent excess production of thyroid hormones. Commonly prescribed medications include methimazole (Tapazole) and propylthiouracil. Improvement in symptoms is gradual and is typically noticeable within 6 to 12 weeks once treatment has started. Treatment may be required for at least a year, sometimes longer. Either medication can result in serious damage to the liver and thus will need to be carefully monitored and not used for extensive periods of time. For many, hyperactivity can be permanently resolved thereafter, others may experience a relapse of symptoms and require further treatment. Signs of allergic reactions to these medications include hives, skin rashes, joint pain and fever.
- Beta-blockers: These medications may be prescribed to target certain symptoms as they are more commonly used to treat hypertension (high blood pressure). The intention is not to reduce thyroid hormone production levels, but rather to alleviate a rapid heart rate and palpitations. Beta-blockers can also treat symptoms of nervousness, agitation and tremor. Side-effects which are common with these medications include headaches, fatigue, dizziness, an upset stomach, diarrhoea or constipation.
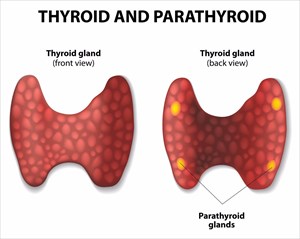
Thyroidectomy: Surgery is an option for pregnant women or those with an inability to tolerate medications or radioactive iodine. A surgeon will remove most of the thyroid gland during the procedure. Risks of surgery involve vocal cord damage, or possible deterioration of the parathyroid glands (four small glands in the neck at the back of thyroid gland, which regulate the level of calcium in the bloodstream). Surgery forms one part of this treatment option, usually requiring lifelong medication doses to assist the body with producing thyroid hormones. Damaged or removed parathyroid glands will also require medication to regulate blood-calcium levels.
- Grave’s ophthalmopathy: Those with diagnosed Grave’s disease that is affecting the eyes can be treated with corticosteroid medications to alleviate swelling behind the eyeballs. Most with mild symptoms can effectively manage symptoms by avoiding bright lights and wind (wearing sunglasses). Cool compresses, lubricating eye drops, and elevating the head while in bed can also help. Severe cases may be corrected with orbital decompression surgery (removal of the bone between the eye socket and sinuses to improve vision and allow more room for bulging eyes to return to their normal position). One of the biggest risks of this surgery is double vision. Another surgical option to correct scar tissue that causes shortening of the eye muscles and results in the eyes being pulled out of alignment is eye muscle surgery. Misaligned eyes can cause double vision. The procedure is performed by cutting the affected muscle away from the eyeball and reattaching it further back. This corrective surgery may require more than one procedure to achieve the desired result.
- Homecare: A doctor may encourage dietary changes to help with improving weight and rectifying muscle wasting. Adding more calories and protein to a daily diet can help. Diet supplementation may only be necessary until an overactive thyroid is under control. A nutritionist may be recommended to assist with meal planning, provide tips for keeping sodium and calcium under control, and also to prevent any unwanted weight gain due to excess calorie consumption. The correct amount of calcium, which can be taken as a supplement can also help to prevent thinning bones or osteoporosis. Vitamin D is also important in the correct doses. A treating doctor can assist with all relevant dietary guidelines during treatment and may also recommend regular exercise, including weight-bearing exercise, to improve the cardiovascular system and overall muscle tone. Exercise is also beneficial for increasing energy levels and reducing excessive appetite.
2. Hypothyroidism treatment
The standard treatment for an underactive thyroid is synthetic thyroid hormone medications (i.e. synthetic thyroxine) taken daily. Taken orally, medication is needed in order to control symptoms of hypothyroidism by restoring balance to hormone levels. Using diagnostic tests, a doctor will determine the correct dosage in order to achieve this. This is important so as to avoid encouraging an underactive thyroid to become overactive by stimulating excess hormone production.
Within a few weeks, daily medication use should begin to take effect and ease symptoms. One of the first signs that the medication is taking effect is the easing off of fatigue and an increase in energy levels. Cholesterol levels will begin to lower and weight that was gained will gradually be reversed.
Treatment with medication is likely to be recommended on a chronic basis (taken for the rest of a person’s life). A doctor will wish to monitor the effects of the medication, and adjust dosages if necessary. Slight adjustment may be required during the initial stages of treatment in order to find the correct balance. Signs that hormone production is in excess include insomnia, increased appetite, shaking or trembling and heart palpitations.
Thyroid-stimulating hormone (TSH) levels are typically checked within 2 to 3 months, and at least once a year thereafter, once treatment commences. A treating doctor will likely discuss medication interactions at the beginning stages of treatment and advise ways to control proper absorption of the drugs being prescribed. Some medications (such as certain antacids), calcium or iron supplements (or multivitamins containing iron) and foodstuffs (such as soy), taken at the same time may interfere with proper absorption of the medication. It is important to take the medication on an empty stomach and avoid eating for 30minutes after taking it.
Severe cases of underactive thyroid, especially if there are signs of coronary artery disease may be treated with low dosages initially, which are gradually increased. This is important so as to allow the heart to slowly adjust to the increased changes in metabolism without adverse effects.
At the correct dose, synthetic thyroid hormone medications do not cause too many side-effects. Those experienced are generally mild. Doses should not be skipped and the medication must not be discontinued without the guidance of the treating doctor. It is not advisable to discontinue taking medication once symptoms ease off as they can then recur. Medication use is designed to keep symptoms under control and restore balance on a lifelong basis.
If a person is diagnosed with Hashimoto’s disease, hormone replacement medications may also be prescribed in order to balance TSH levels and help to relieve symptoms, stabilising a person’s condition adequately. There is, however, no known cure for this disease. Surgery is another treatment option in severe cases where the disease is in advanced stages (this involves removal of part or all of the thyroid gland).
Homecare advice a doctor may recommend may include the following:
- Foods to avoid: Soy (phytoestrogens interfere with enzymes needed for the production of thyroid hormones), iodine-rich foods and iodised salt (these can suppress activity of the thyroid gland), and high-fibre foodstuffs eaten in excess (this interferes with medication absorption), Vegetables such as broccoli, spinach, kale, cabbage and Brussels sprouts can also interfere with medication absorption and should be limited in a daily diet. Alcohol and caffeine consumption, as well as use of tobacco can also influence the effectiveness of medication and should be kept to a minimum or avoided altogether.
- Foods to eat: Blueberries, bell peppers and tomatoes are rich in antioxidants which assist with thyroid function, as well as improve overall state of health. Whole grains, foodstuffs rich in vitamin B, small amounts of selenium found in sunflower seeds and Brazil nuts, and those containing tyrosine, such as meats, legumes and dairy products can all benefit the function of the thyroid.
- Exercise activity: To help combat fatigue, depression, joint aches and pains, reduced metabolism, weight gain or heart palpitations, exercise activity can help, as well as improve overall cardiovascular health and muscle mass too. To strengthen the cardiovascular system, aerobic exercise activity, such as brisk walking, jogging (or running) and sporting activities (such as soccer or tennis), in combination with strength training, can help to prevent ventricular arrhythmias and a rapid heartbeat from developing, whilst also building muscle. Added benefits include improved mood and less fatigue. Low-impact exercise is also beneficial and can include walking, Pilates, yoga, swimming or biking. If muscle and joint pain are problematic, these types of exercises can help to improve and minimise strain on the body’s joints, especially those in the back, knees or hips.
Before a diet or exercise regimen is adjusted, a treating doctor should be consulted. Diet and exercise are not a substitute for medication treatment but can certainly help in maintaining an adequate state of health. Some individuals may experience some discomfort with exercise, and thus should perhaps avoid certain activities and incorporate others which may be more beneficial. A doctor can also best advise when it comes to eating habits, particularly when it comes to certain diet preferences, such as vegetarianism, or those with known food allergies.
It is best to talk to a treating doctor before making any diet and exercise adjustments or including the use of any supplements. Lifestyle changes can have an influence on the function of the thyroid gland, affecting metabolism as well.
As with every treatment, adherence to medication is key in making the medication work as intended. If you're just starting thyroid medication, here's what to expect.
3. Goitres (Goiters) / thyroid nodules / malignant nodules (thyroid cancer) treatment
Goitres are not always a serious cause for concern and are often only treated when they are the source of severe symptoms. Treatment measures may include the following:
- Wait and watch: Small goitres or benign thyroid nodules that are not causing any symptomatic problems may merely be monitored. Provided the thyroid gland is functioning normally, treatment may not be required. Periodic checks, thyroid function tests or a biopsy may be recommended on a frequent basis. If any abnormalities or changes are detected, a doctor will wish to assess potential growth of a goitre or nodule.
- Medications: Drugs to stabilise or restore thyroid hormone production may be necessary in the case of an overactive or underactive thyroid. In the case of hypothyroidism, medications can be used to slow the secretion of TSH in order to reduce the size of the goitre or nodule. Corticosteroids or aspirin may also be recommended to treat signs of inflammation. Radioactive iodine may be recommended in the case of hyperthyroidism and may be prescribed to be taken orally. The medication can help to reduce the size of a goitre or nodule as well.
- Surgery (near-total thyroidectomy): Large, bothersome goitres or nodules (whether benign or malignant) may be removed with a partial or total thyroidectomy, especially where the growth affects ability to swallow or breathe comfortably. A doctor may perform a biopsy to determine the need for removal (or treatment to shrink the growth using medication). Surgery is also a recommended means of treatment in the case of thyroid cancer and can sometimes involve the removal of lymph nodes in the neck (if affected by cancer spreading), as well as a thyroid lobectomy (partial removal of the thyroid gland tissue on one side / lobe). Medications may likely be prescribed following any surgical procedure, depending on how much of the thyroid gland has been removed.
- Other therapies and treatments (malignant nodules and tumours): Thyroid cancer (malignancy) may involve radiation therapy (alone or along with surgery). External radiation therapy can be used to target high-energy beams (X-rays and protons) at precise points in the body for just a few minutes at a time, several times a week (for several weeks). This therapy may be recommended for those who are not good candidates for surgery or if spreading of the cancer occurs despite other treatment measures, especially if there is an increased risk for recurrence. If it is determined that thyroid cancer has spread to other portions of the body, chemotherapy may be recommended to treat the condition. Chemotherapy is not normally the go-to treatment option for thyroid cancer, but may be beneficial if a person has not responded well to other treatment options. A cancerous goitre or nodule may also be treated with alcohol ablation, whereby a small amount of alcohol is injected into the growth using an ultrasound to guide a doctor in determining the precise location of the growth. This may be recommended if the growth is not easily accessible for removal via surgical means or if the cancer is limited to a small area. Targeted drug therapy (medications) and palliative care may also be recommended in the case of thyroid cancer.
- Homecare: A doctor may recommend controlled iodine intake by incorporating iodised salt, seaweed (sushi) and seafood (shellfish or shrimp), some dairy products and fruits and vegetables into a diet. Some may have excess iodine in the system and in this instance control by restriction may be necessary and involve avoiding iodine containing supplements and certain foodstuffs.

 Thyroidectomy:
Thyroidectomy: